Electrocardiographic findings in COVID-19: analysis of tele-ECGs in Moscow ECG IT Center
- Authors: Taskina V.Y.1, Demkina A.E.1, Gazashvili T.M.2, Shkoda A.S.2, Vladzymyrskyy A.V.3,4, Morozov S.P.1
-
Affiliations:
- Research and Practical Clinical Center for Diagnostics and Telemedicine Technologies of the Moscow Healthcare Department
- L.A. Vorokhobov City Clinical Hospital No. 67 of the Moscow Healthcare Department
- Moscow Center for Diagnostics and Telemedicine
- The First Sechenov Moscow State Medical University (Sechenov University)
- Issue: Vol 2, No 3 (2021)
- Pages: 235-248
- Section: Original Study Articles
- URL: https://journals.rcsi.science/DD/article/view/71885
- DOI: https://doi.org/10.17816/DD71885
- ID: 71885
Cite item
Abstract
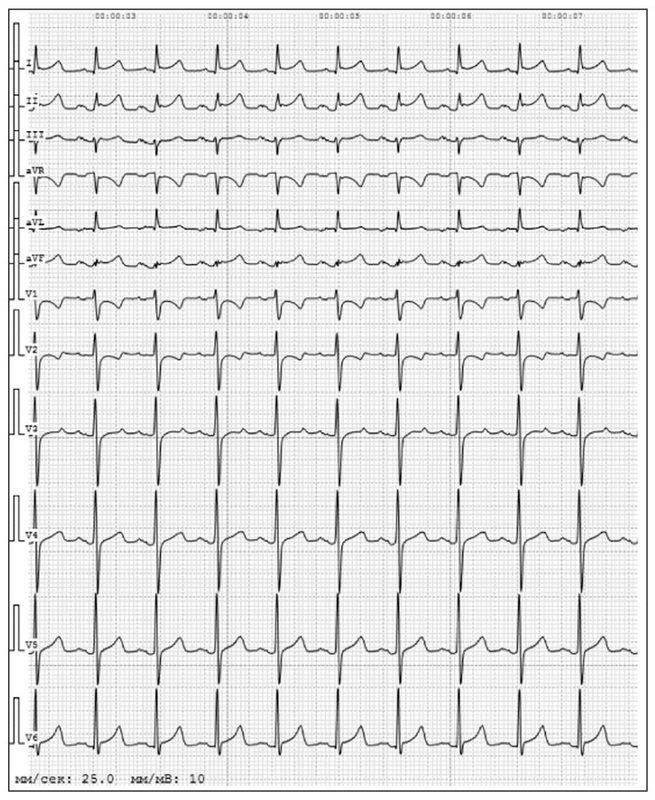
BACKGROUND: Coronavirus disease (COVID-19) affects the cardiovascular system and the primary damage to the respiratory system involved in the pathological process. However, in the available literature, the electrocardiography (ECG) analyses are based only on small-sample studies and case reports, which determine the relevance of larger-scale studies to clarify the nature and prevalence of ECG abnormalities in subjects with confirmed coronavirus infection.
AIM: To determine the distribution of ECG changes in COVID-19 patients representing a non-selective population of Moscow residents.
MATERIALS AND METHODS: We performed a retrospective analysis of ECGs from 42,799 patients from March 10, 2020 to March 10, 2021 with a verified diagnosis of COVID-19 was performed. The study included patients admitted to Moscow clinical hospitals connected to the ECG IT Center. A standard 12-lead ECG was obtained and transmitted via an Internet connection to the server of the ECG IT Center, where the ECG interpretation was performed.
RESULTS: ECG changes were detected in 54% of patients. The most common cardiac arrhythmias were supraventricular extrasystole (12.6%) and atrial fibrillation (12.0%) reported in patients. Signs of the overloaded right heart were detected in 12.5% of cases, of which the ECG pattern of pulmonary embolism was confirmed in 485 patients (1.13%). Infarction ECG pattern was observed in 4.5% of patients, among which 3 cases of Brugada ECG pattern were reported. The incidence of ST-T changes was 2.2% of all study patients. Prolonged QT and QTc intervals were recorded in 540 patients (1.26%). In addition, individual cases of ventricular fibrillation, Frederick syndrome, and atrioventricular block of various degrees were reported.
CONCLUSION: The distribution of incidence of ECG changes in COVID-19 was shown based on the data obtained. The high incidence of atrial fibrillation, which is a risk factor for thromboembolic complications, was confirmed. Moreover, a significant prevalence of ECG patterns of overloaded right heart was shown, some are associated with pulmonary embolism. Other reported ECG changes were characterized by a significantly lower prevalence, which does not reduce their clinical significance. The data obtained may be used to improve COVID-19 patient management strategy in the future.
Full Text
##article.viewOnOriginalSite##About the authors
Varvara Y. Taskina
Research and Practical Clinical Center for Diagnostics and Telemedicine Technologies of the Moscow Healthcare Department
Email: varvara.taskina@gmail.com
ORCID iD: 0000-0003-4452-7667
SPIN-code: 6314-8190
MD, Cand. Sci. (Med.), Researcher, Telemedicine Research Projects Sector
Russian Federation, 24 bld.1, Petrovka street, Moscow, 127051Alexandra E. Demkina
Research and Practical Clinical Center for Diagnostics and Telemedicine Technologies of the Moscow Healthcare Department
Email: a.demkina@npcmr.ru
ORCID iD: 0000-0001-8004-9725
SPIN-code: 4657-5501
MD, Cand. Sci. (Med.), Head of the Telemedicine Research Projects Sector
Russian Federation, 24 bld.1, Petrovka street, Moscow, 127051Tamara M. Gazashvili
L.A. Vorokhobov City Clinical Hospital No. 67 of the Moscow Healthcare Department
Email: tamaradoc24@gmail.com
ORCID iD: 0000-0002-5875-9699
SPIN-code: 4208-2303
MD, Head of the Center for Diagnostic Investigations
Russian Federation, 2/44, Salyama Adilya street, 123423 MoscowAndrey S. Shkoda
L.A. Vorokhobov City Clinical Hospital No. 67 of the Moscow Healthcare Department
Email: a.shkoda@67gkb.ru
ORCID iD: 0000-0002-9783-1796
SPIN-code: 4520-2141
MD, Dr. Sci. (Med.), Professor, Chief Physician
Russian Federation, 2/44, Salyama Adilya street, 123423 MoscowAnton V. Vladzymyrskyy
Moscow Center for Diagnostics and Telemedicine; The First Sechenov Moscow State Medical University (Sechenov University)
Author for correspondence.
Email: a.vladzimirsky@npcmr.ru
ORCID iD: 0000-0002-2990-7736
SPIN-code: 3602-7120
MD, Dr. Sci. (Med.), Deputy Director for Science; professor of the Department of Information and Internet Technologies
Russian Federation, 24 bld.1, Petrovka street,127051 Moscow; 8 bld.2, Trubetskaya street, 119991 MoscowSergey P. Morozov
Research and Practical Clinical Center for Diagnostics and Telemedicine Technologies of the Moscow Healthcare Department
Email: morozov@npcmr.ru
ORCID iD: 0000-0001-6545-6170
SPIN-code: 8542-1720
MD, Dr. Sci. (Med.), Professor
Russian Federation, 24 bld.1, Petrovka street, Moscow, 127051References
- Wu Z, McGoogan JM. Characteristics of and important lessons from the Coronavirus Disease 2019 (COVID-19) outbreak in China: summary of a report of 72314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020;323(13):1239–1242. doi: 10.1001/jama.2020.2648
- Shi S, Qin M, Shen B, et al. Association of cardiac injury with mortality in hospitalized patients with COVID-19 in wuhan, China. JAMA Cardiol. 2020;5(7):802–810. doi: 10.1001/jamacardio.2020.0950
- Madjid M, Safavi-Naeini P, Solomon SD, Vardeny O. Potential effects of coronaviruses on the cardiovascular system: a review. JAMA Cardiol. 2020;5(7):831–840. doi: 10.1001/jamacardio.2020.1286
- Vidovich MI. Transient Brugada-like electrocardiographic pattern in a patient with COVID-19. JACC Case Rep. 2020;2(9):1245–1249. doi: 10.1016/j.jaccas.2020.04.007
- Gérard A, Romani S, Fresse A, et al. "Off-label" use of hydroxychloroquine, azithromycin, lopinavir-ritonavir and chloroquine in COVID-19: A survey of cardiac adverse drug reactions by the French Network of Pharmacovigilance Centers. Therapie. 2020;75(4):371–379. doi: 10.1016/j.therap.2020.05.002
- Mai F, Del Pinto R, Ferri C. COVID-19 and cardiovascular diseases. J Cardiol. 2020;76(5):453–458. doi: 10.1016/j.jjcc.2020.07.013
- Ryabykina GV. ECG changes in COVID-19. Kardiologiia. 2020; 60(8):16–22. (In Russ). doi: 10.18087/cardio.2020.8.n1192
- Poteshkina NG, Lysenko MA, Kovalevskaya EA, et al. Cardiac damage in patients with COVID-19 coronavirus infection. Arterial Hypertension. 2020;26(3):277–287. (In Russ). doi: 10.18705/1607-419X-2020-26-3-277-287
- Lanza GA, De Vita A, Ravenna SE, et al. Electrocardiographic findings at presentation and clinical outcome in patients with SARS-CoV-2 infection. Europace. 2021;23(1):123–129. doi: 10.1093/europace/euaa245
- Morozov SP, Vladzimirskyy AV, Demkina AE, et al. Centralization of descriptions of electrocardiographic studies in primary health care: guidelines. The series "Best practices of radiation and instrumental diagnostics". Issue 62. Moscow: Scientific and Practical Clinical Center for Diagnostics and Telemedicine Technologies of the Department of Healthcare of the City of Moscow; 2020. 24 p. (In Russ).
- Morozov SP, Vladzimirskyy AV, Simenyura SS, et al. Digitalization of primary functional diagnostics data (example of electrocardiographic studies). Creative Cardiology. 2020;14(1):16–23. doi: 10.24022/1997-3187-2020-14-1-16-23
- Li Y, Liu T, Tse G, et al. Electrocardiograhic characteristics in patients with coronavirus infection: A single-center observational study. Ann Noninvasive Electrocardiol. 2020;25:e12805. doi: 10.1111/anec.12805
- Bertini M, Ferrari R, Guardigli G, et al. Electrocardiographic features of 431 consecutive, critically ill COVID-19 patients: An insight into the mechanisms of cardiac involvement. Europace. 2020;22(12):1848–1854. doi: 10.1093/europace/euaa258
- Angeli F, Spanevello A, De Ponti R, et al. Electrocardiographic features of patients with COVID-19 pneumonia. Eur J Intern Med. 2020;78:101–106. doi: 10.1016/j.ejim.2020.06.015
- Demkina AE, Morozov SP, Vladzymyrskyy AV, et al. Risk factors for outcomes of COVID-19 patients: an observational study of 795572 patients in Russia. medRxiv. 2020;11.02.20224253. doi: 10.1101/2020.11.02.20224253
- Atrial fibrillation and flutter. Clinical guidelines (approved by the Ministry of Health of the Russian Federation). 2020. Available from: https://scardio.ru/content/Guidelines/2020/Clinic_rekom_FP_TP.pdf. Accessed: 21.05.2021.
- Hu YF, Cheng WH, Hung Y, et al. Management of atrial fibrillation in COVID-19 pandemic. Circ J. 2020;84(10):1679–1685. doi: 10.1253/circj.CJ-20-0566
- Wang Y, Chen L, Wang J, et al. Electrocardiogram analysis of patients with different types of COVID-19. Ann Noninvasive Electrocardiol. 2020;25(6):e12806. doi: 10.1111/anec.12806
- Wang D, Hu B, Hu C, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in wuhan, China [published correction appears in JAMA. 2021 Mar 16;325(11):1113]. JAMA. 2020;323(11):1061–1069. doi: 10.1001/jama.2020.1585
- Shlyakhto EV, Parmon EV, Berngardt ER, Zhabina ES. Features of electrocardiographic changes in non-coronarogenic syndromes in patients with COVID-19. Russian Journal of Cardiology. 2020; 25(7):4019. (In Russ). doi: 10.15829/1560-4071-2020-4019.
Supplementary files