Patient dose monitoring software in radiology
- Autores: Shatenok M.P.1, Ryzhov S.A.1,2, Lantukh Z.A.1, Druzhinina Y.V.1,3, Tolkachev K.V.1
-
Afiliações:
- Research and Practical Clinical Center for Diagnostics and Telemedicine Technologies
- Dmitry Rogachev National Medical Research Center of Pediatric Hematology, Oncology and Immunology
- Russian Medical Academy of Continuous Professional Education
- Edição: Volume 3, Nº 3 (2022)
- Páginas: 212-230
- Seção: Reviews
- URL: https://journals.rcsi.science/DD/article/view/106083
- DOI: https://doi.org/10.17816/DD106083
- ID: 106083
Citar
Resumo
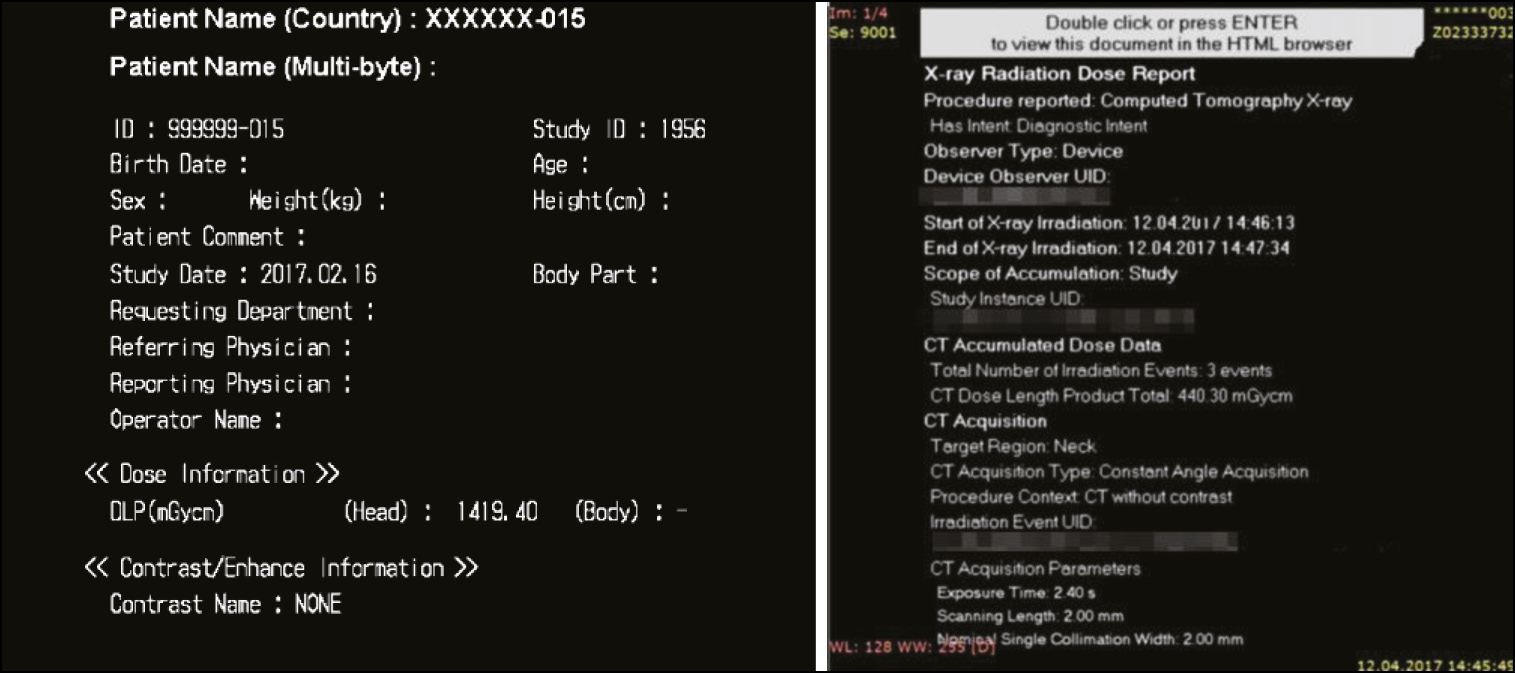
An increase in the number of diagnostic procedures using ionizing radiation (computed tomography, interventional procedures, and the use of nuclear medicine) results in an increase in radiation exposure and, consequently, an increase in collective and individual doses of radiation to patients.
Diagnostic studies from the international professional community are extensively focusing on issues such as management and dose optimization. Worldwide practice can resolve these issues using software for monitoring patient doses to automatically collect, analyze, and account for patient doses in various types of diagnostic studies. The software allows to obtain data on the doses of patients from X-ray procedures and detailed information about studies, track the total accumulated dose of the patient, and maintain statistics on the device, X-ray laboratory, and the medical organization. It also helps analyze the collected dosimetric data, deduce the causal relationship between dose indications and diagnostic procedure conditions, and monitor the effectiveness of the equipment.
The basic capabilities of patient dose monitoring software (DMS) available on the global market were investigated. The major technical requirements for the software functional needed in practical work were defined.
Modern DMS have a wide range of possibilities for automated collection, storage, and management of patient radiation exposure data in radiology departments. DMS increase the quality of healthcare services, provide patient safety, and optimize the workflow of medical organizations.
Palavras-chave
Texto integral
##article.viewOnOriginalSite##Sobre autores
Maria Shatenok
Research and Practical Clinical Center for Diagnostics and Telemedicine Technologies
Email: maria.prusova@gmail.com
ORCID ID: 0000-0001-9217-7011
Código SPIN: 5165-7113
Rússia, Moscow
Sergey Ryzhov
Research and Practical Clinical Center for Diagnostics and Telemedicine Technologies; Dmitry Rogachev National Medical Research Center of Pediatric Hematology, Oncology and Immunology
Email: s.ryzhov@npcmr.ru
ORCID ID: 0000-0002-0640-7368
Código SPIN: 6595-4011
Rússia, Moscow; Moscow
Zoya Lantukh
Research and Practical Clinical Center for Diagnostics and Telemedicine Technologies
Email: z.lantukh@npcmr.ru
ORCID ID: 0000-0001-6623-9610
Código SPIN: 5486-6496
Rússia, Moscow
Yuliya Druzhinina
Research and Practical Clinical Center for Diagnostics and Telemedicine Technologies; Russian Medical Academy of Continuous Professional Education
Email: yu.druzhinina@npcmr.ru
ORCID ID: 0000-0002-3230-3722
Código SPIN: 1973-2848
Rússia, Moscow; Moscow
Kirill Tolkachev
Research and Practical Clinical Center for Diagnostics and Telemedicine Technologies
Autor responsável pela correspondência
Email: k.tolkachev@npcmr.ru
ORCID ID: 0000-0001-8871-8700
Código SPIN: 3196-7497
Rússia, Moscow
Bibliografia
- Parakh A, Kortesniemi M, Schindera ST. CT radiation dose management: a comprehensive optimization process for improving patient safety. Radiology. 2016;280(3):663–673. doi: 10.1148/radiol.2016151173
- Druzhinina YV, Ryzhov SA, Vodovatov AV, et al. COVID-19: changes in CT radiation burden across Moscow medical facilities. Digital Diagnostics. 2022;3(1):5–15. (In Russ). doi: 10.17816/DD87628
- Morozov SP, Soldatov IV, Lantukh ZA, et al. Characteristics of the dose load on patients in medical organizations in Moscow [Internet]. (In Russ). Available from: https://www.elibrary.ru/item.asp?id=42395967. Accessed: 15.03.2022.
- Rehani MM, Yang K, Melick ER, et al. Patients undergoing recurrent CT scans: assessing the magnitude. Eur Radiol. 2020;30(4):1828–1836. doi: 10.1007/s00330-019-06523-y
- Brenner DJ, Hall EJ. Computed tomography an increasing source of radiation exposure. N Engl J Med. 2007;357(22):2277–2284. doi: 10.1056/NEJMra072149
- Pasov VV, Korotkov VA. Surgical treatment of early radiation ulcer formed after endovascular intervention. Radiation Risk. 2020;29(4):158–163. (In Russ). doi: 10.21870/0131-3878-2020-29-4-158-163
- Ivanov VA, Belyakin SA, Permyakov SV, et al. Local radiation damage to the skin and thoracic vertebrae after endovascular angioplasty of the coronary arteries. Diagnostic Int Radiol. 2010;29(4):73–76. (In Russ).
- Ryzhov SA. Radiation accidents and errors in medicine. Terms and definitions. Med Physics. 2019;81(1):73–90. (In Russ).
- European Commission. Council Directive 2013/59/EURATOM of December 5, 2013 laying down basic safety standards for protection against the dangers arising from exposure to ionising radiation, and repealing Directives 89/618/Euratom, 90/641/Euratom, 96/29/Euratom, 97/43/Euratom and 2003/122/Euratom. OJ of the EU. 2014;13(57):1–80. Available from: http://eur-lex.europa.eu/eli/dir/2013/59/oj. Accessed: 15.03.2022.
- Loose RW, Vano E, Mildenberger P, et al. Radiation dose management systems-requirements and recommendations for users from the ESR EuroSafe Imaging initiative. Eur Radiol. 2021;31(4):2106–2114. doi: 10.1007/s00330-020-07290-x
- Lantukh ZA, Druzhinina YuV, Vodovatov AV, et al. The use of reference diagnostic levels for adult patients in radiation diagnostics. Ed. by S.P. Morozov. Vol. 86. Moscow: Research and Practical Clinical Center for Diagnostics and Telemedicine Technologies; 2020. 36 p. (Series: Best practices of radiation and Instrumental diagnostics) (In Russ).
- Vañó E, Miller DL, Martin CJ, et al. ICRP Publication 135: diagnostic reference levels in medical imaging. Ann ICRP. 201746(1):1–144. doi: 10.1177/0146645317717209
- Anonymous, Size-specific Dose Estimates (SSDE) in Pediatric and Adult Body CT examinations. In: American Association of Physicists in Medicine, TG-204. MD: AAPM; 2011.
- Habibzadeh MA, Ay MR, Asl AR, et al. Impact of miscentering on patient dose and image noise in x-ray CT imaging: phantom and clinical studies. Phys Med. 2012;28(3):191–199. doi: 10.1016/j.ejmp.2011.06.002
- Barreto I, Lamoureux R, Olguin C, et al. Impact of patient centering in CT on organ dose and the effect of using a positioning compensation system: Evidence from OSLD measurements in postmortem subjects. J Appl Clin Med Phys. 2019;20(6):141–151. doi: 10.1002/acm2.12594
- Xu XG. An exponential growth of computational phantom research in radiation protection, imaging, and radiotherapy: a review of the fifty-year history. Phys Med Biol. 2014;59(18):R233–R302. doi: 10.1088/0031-9155/59/18/R233
- Iriuchijima A, Fukushima Y, Ogura A. Comparison of organ dose calculation using monte carlo simulation and in-phantom dosimetry in CT examination. Nihon Hoshasen Gijutsu Gakkai Zasshi. 2018;74(2):166–171. doi: 10.6009/jjrt.2018_JSRT_74.2.166
- Fitousi N. Patient dose monitoring systems: a new way of managing patient dose and quality in the radiology department. Phys Med. 2017;44:212–221. doi: 10.1016/j.ejmp.2017.06.013
- Tsalafoutas IA, Hassan Kharita M, Al-Naemi H, Kalra MK. Radiation dose monitoring in computed tomography: status, options and limitations. Phys Med. 2020;79:1–15. doi: 10.1016/j.ejmp.2020.08.020
- Heilmaier C, Zuber N, Bruijns B, et al. Implementation of dose monitoring software in the clinical routine: first experiences. Rofo. 2016;188(1):82–88. doi: 10.1055/s-0041-106071
- Nicol RM, Wayte SC, Bridges AJ, Koller CJ. Experiences of using a commercial dose management system (GE DoseWatch) for CT examinations. Br J Radiol. 2016;89(1057):20150617. doi: 10.1259/bjr.20150617
Arquivos suplementares