Volumetry versus linear diameter lung nodule measurement: an ultra-low-dose computed tomography lung cancer screening study
- Авторлар: Suchilova M.M.1, Blokhin I.A.1, Aleshina O.O.2, Gombolevskiy V.A.3, Reshetnikov R.V.1, Bosin V.Y.1, Omelyanskaya O.V.1, Vladzymyrskyy A.V.1,4
-
Мекемелер:
- Moscow Center for Diagnostics and Telemedicine
- City Clinical Hospital No 13
- Artificial Intelligence Research Institute
- The First Sechenov Moscow State Medical University (Sechenov University)
- Шығарылым: Том 4, № 1 (2023)
- Беттер: 5-13
- Бөлім: Original Study Articles
- URL: https://journals.rcsi.science/DD/article/view/146871
- DOI: https://doi.org/10.17816/DD117481
- ID: 146871
Дәйексөз келтіру
Аннотация
BACKGROUND: The Dutch–Belgian Randomized Lung Cancer Screening Trial (NELSON) used a volume-based protocol and significantly reduced the prevalence of false-positive results (2.1%).
AIM: To compare the performance of manual linear diameter and semi-automated volumetric nodule measurement in the pilot project “Moscow Lung Cancer Screening” ultra-low-dose computed tomography pilot study.
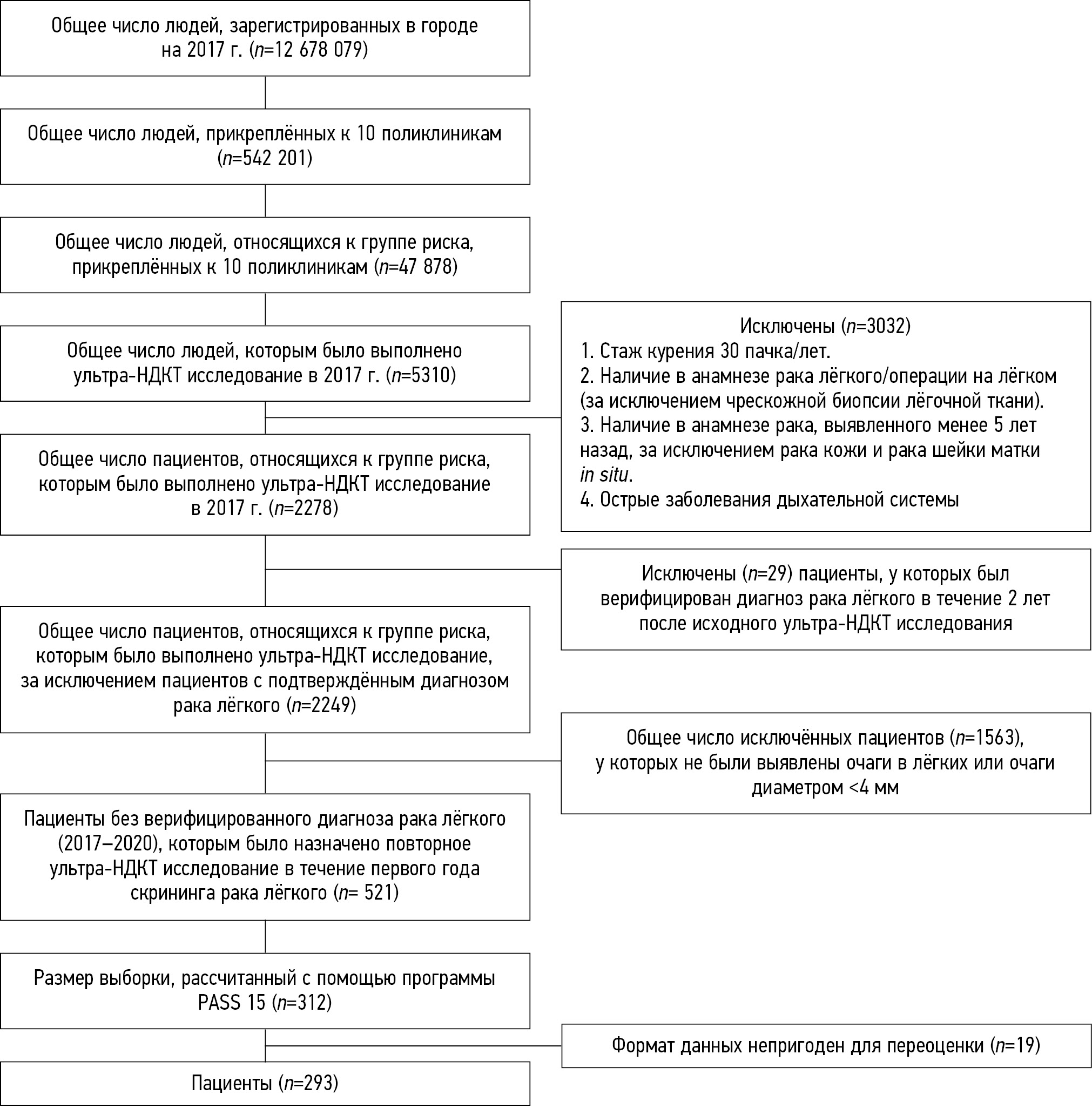
MATERIALS AND METHODS: The study included individuals with a lung nodule of at least 4 mm on baseline-computed tomography of the Moscow lung cancer screening between February 2017 and February 2018, without verified lung cancer diagnosis until 2020. The radiation dose was selected individually and did not exceed 1 mSv. All scans were assessed by three blinded readers to measure the maximum and minimum transversal nodule diameter and extrapolated volume. As a reference value of size and volume, the average value from the results of expert measurements was obtained. A false-positive nodule was defined as a nodule <6 mm/<100 mm3 and a false-negative nodule as a nodule ≥6 mm/≥100 mm3.
RESULTS: Overall, 293 patients were included (166 men; mean age, 64.6 ± 5.3years); 199 lung nodules were <6 mm/<100 mm3 and 94 were ≥6 mm/≥100 mm3. Regarding volumetric measurements, 32 [10.9%; 4 false-positive, 28 false-negative], 29 [9.9%; 17 false-positive, 12 false-negative], and 30 [10.2%; 6 false-positive, 24 false-negative] nodule discrepancies were reported by readers 1, 2, and 3 respectively. For linear diameter measurement, 92 [65.5%; 107 false-positive, 85 false-negative], 146 [49.8%; 58 false-positive, 88 false-negative], and 102 [34.8%; 23 false-positive, 79 false-negative] nodule discrepancies were reported by readers 1, 2, and 3 respectively.
CONCLUSIONS: The use of lung nodule volumetry strongly reduces the number of false-positive and false-negative nodules compared with nodule diameter measurements, in an ultra-low-dose computed tomography lung cancer screening program.
Негізгі сөздер
Толық мәтін
##article.viewOnOriginalSite##Авторлар туралы
Maria Suchilova
Moscow Center for Diagnostics and Telemedicine
Хат алмасуға жауапты Автор.
Email: m.suchilova@npcmr.ru
ORCID iD: 0000-0003-1117-0294
SPIN-код: 4922-1894
MD
Ресей, MoscowIvan Blokhin
Moscow Center for Diagnostics and Telemedicine
Email: i.blokhin@npcmr.ru
ORCID iD: 0000-0002-2681-9378
SPIN-код: 3306-1387
MD
Ресей, MoscowOlga Aleshina
City Clinical Hospital No 13
Email: olya.aleshina.tula@gmail.com
ORCID iD: 0000-0001-9924-0204
SPIN-код: 6004-2422
MD
Ресей, MoscowVictor Gombolevskiy
Artificial Intelligence Research Institute
Email: gombolevskiy@npcmr.ru
ORCID iD: 0000-0003-1816-1315
SPIN-код: 6810-3279
MD, Cand. Sci. (Med)
Ресей, MoscowRoman Reshetnikov
Moscow Center for Diagnostics and Telemedicine
Email: reshetnikov@fbb.msu.ru
ORCID iD: 0000-0002-9661-0254
SPIN-код: 8592-0558
Cand. Sci. (Phys.-Math.)
Ресей, MoscowViktor Bosin
Moscow Center for Diagnostics and Telemedicine
Email: bosin@npcmr.ru
ORCID iD: 0000-0002-4619-2744
SPIN-код: 3380-7889
MD, Dr. Sci. (Med.)
Ресей, MoscowOlga Omelyanskaya
Moscow Center for Diagnostics and Telemedicine
Email: o.omelyanskaya@npcmr.ru
ORCID iD: 0000-0002-0245-4431
SPIN-код: 8948-6152
Ресей, Moscow
Anton Vladzymyrskyy
Moscow Center for Diagnostics and Telemedicine; The First Sechenov Moscow State Medical University (Sechenov University)
Email: a.vladzimirskiy@npcmr.ru
ORCID iD: 0000-0002-2990-7736
SPIN-код: 3602-7120
MD, Dr. Sci (Med.)
Ресей, Moscow; MoscowӘдебиет тізімі
- De Koning HJ, van der Aalst CM, de Jong PA, et al. Reduced lung-cancer mortality with volume CT screening in a randomized trial. N Engl J Med. 2020;382(6):503–513. doi: 10.1056/NEJMoa1911793
- Henschke CI, Boffetta P, Yankelevitz DF, Altorki N. Computed tomography screening: The International Early Lung Cancer Action Program Experience. Thoracic Sur Clin. 2015;25(2):129–143. doi: 10.1016/j.thorsurg.2014.12.001
- Callister ME, Baldwin DR, Akram AR, et al. Correction: British Thoracic Society guidelines for the investigation and management of pulmonary nodules: Accredited by NICE. Thorax. 2015;70(Suppl 2):ii1–ii54. doi: 10.1136/thoraxjnl-2015-207168
- Oudkerk M, Devaraj A, Vliegenthart R, et al. European Position Statement on Lung Cancer Screening. Lancet Oncology. 2017;18(12):e754–766. doi: 10.1016/S1470-2045(17)30861-6
- Wood DE, Kazerooni EA, Baum SL, et al. Lung cancer screening, version 3.2018, NCCN clinical practice guidelines in oncology. J Natl Compr Canc Netw. 2018;16(4):412–441. doi: 10.6004/jnccn.2018.0020
- Horeweg N, Scholten ET, de Jong PA, et al. Detection of lung cancer through low-dose CT screening (NELSON): A prespecified analysis of screening test performance and interval cancers. Lancet Oncology. 2014;15(3):1342–1350. doi: 10.1016/S1470-2045(14)70387-0
- Oudkerk M, Liu S, Heuvelmans MA, et al. Lung cancer LDCT screening and mortality reduction: Evidence, pitfalls and future perspectives. Nat Rev Clin Oncol. 2021;18(3):135–151. doi: 10.1038/s41571-020-00432-6
- Duffy SW, Field JK. Mortality reduction with low-dose CT screening for lung cancer. N Engl J Med. 2020;382(6):572–573. doi: 10.1056/NEJMe1916361
- Morozov SP, Kuzmina ES, Vetsheva NN, et al. Moscow screening: Screening of lung cancer using low-dose computed tomography. Problems Social Hygiene Healthcare History Med. 2019;27(S):630–636. (In Russ). doi: 10.32687/0869-866X-2019-27-si1-630-636
- Gombolevsky VA, Barchuk AA, Laipan AS, et al. Lung сancer screening with low-dose computed tomography: Management and efficiency. Radiology Practice. 2018;(1):28–36. (In Russ).
- Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33(1):159–174.
- Revel MP, Bissery A, Bienvenu M, et al. Are two-dimensional ct measurements of small noncalcified pulmonary nodules reliable? Radiology. 2004;231(2):453–458. doi: 10.1148/radiol.2312030167
- Xie X, Willemink MJ, Zhao Y, et al. Inter- and intrascanner variability of pulmonary nodule volumetry on low-dose 64-row CT: an anthropomorphic phantom study. BJR. 2013;86(1029):20130160. doi: 10.1259/bjr.20130160
- Kulberg NS, Reshetnikov RV, Novik VP, et al. Inter-observer variability between readers of CT images: all for one and one for all. Digital Diagnostics. (In Russ). 2021;2(2):105–118 doi: 10.17816/DD60622
Қосымша файлдар