根据通过低剂量计算机断层扫描的肺癌筛查数据对肺部病灶线性尺寸和体积进行的测量比较
- 作者: Suchilova M.M.1, Blokhin I.A.1, Aleshina O.O.2, Gombolevskiy V.A.3, Reshetnikov R.V.1, Bosin V.Y.1, Omelyanskaya O.V.1, Vladzymyrskyy A.V.1,4
-
隶属关系:
- Moscow Center for Diagnostics and Telemedicine
- City Clinical Hospital No 13
- Artificial Intelligence Research Institute
- The First Sechenov Moscow State Medical University (Sechenov University)
- 期: 卷 4, 编号 1 (2023)
- 页面: 5-13
- 栏目: 原创性科研成果
- URL: https://journals.rcsi.science/DD/article/view/146871
- DOI: https://doi.org/10.17816/DD117481
- ID: 146871
如何引用文章
详细
论证。根据荷兰-比利时NELSON肺癌筛查研究,病灶的体积测量(容量分析法)可以将假阳性结果的发生率降低到2.1%。
目的是根据莫斯科肺癌筛查试点项目的数据通过低剂量计算机断层扫描对人工病灶线性尺寸测量与半自动病灶体积测量的诊断准确性和一致性进行比较。
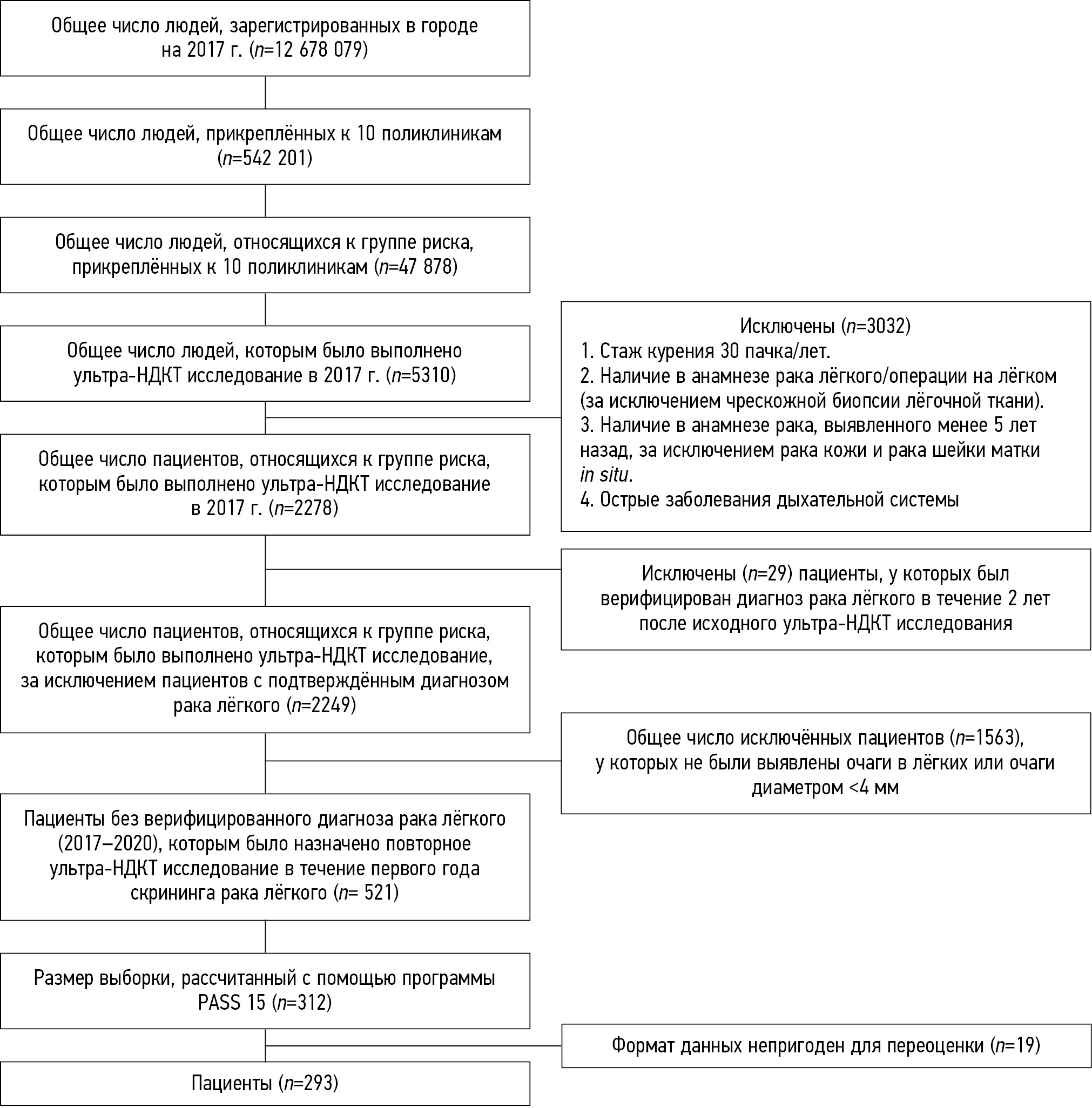
材料和方法。293名在2020年前没有被核实诊断为肺癌的患者被纳入筛查计划,他们在2017年2月至2018年2月时间内接受了一次低剂量计算机断层扫描,显示肺部结节的大小至少为4毫米。辐射负载是个性化的,不超过1毫西弗。所有低剂量计算机断层扫描图像都由三位专家独立评估,以测量病灶的长轴以及外推体积。从专家测量得到的尺寸和体积的平均值作为参考值。<6毫米/<100毫米3 的病灶视为假阳性,≥6毫米/≥100毫米3 的病灶视为假阴性。
结果。293名患者(166名男性;56%;平均年龄为64.6±5.3岁)被纳入研究。共有199个<6毫米/<100毫米3 的肺部病灶。专家1、2和3分别记录了32个[10.9%;4个假阳性,28个假阴性]、29个[9.9%;17个假阳性,12个假阴性]和30个[10.2%。6个假阳性,24个假阴性]的病灶的体积测量与参考标准的差异,以及分别记录了92个[65.5%;107个假阳性,85个假阴性]、146个[49.8%;58个假阳性,88个假阴性]和102个[34.8%;23个假阳性,79个假阴性]病灶的线性尺寸测量与参考标准的差异。
结论。在低剂量计算机断层扫描肺癌筛查项目中,与病灶的线性大小的测量相比,使用肺部病灶的容积测定法可显著减少假阳性和假阴性结果的数量。
作者简介
Maria M. Suchilova
Moscow Center for Diagnostics and Telemedicine
编辑信件的主要联系方式.
Email: m.suchilova@npcmr.ru
ORCID iD: 0000-0003-1117-0294
SPIN 代码: 4922-1894
MD
俄罗斯联邦, MoscowIvan A. Blokhin
Moscow Center for Diagnostics and Telemedicine
Email: i.blokhin@npcmr.ru
ORCID iD: 0000-0002-2681-9378
SPIN 代码: 3306-1387
MD
俄罗斯联邦, MoscowOlga O. Aleshina
City Clinical Hospital No 13
Email: olya.aleshina.tula@gmail.com
ORCID iD: 0000-0001-9924-0204
SPIN 代码: 6004-2422
MD
俄罗斯联邦, MoscowVictor A. Gombolevskiy
Artificial Intelligence Research Institute
Email: gombolevskiy@npcmr.ru
ORCID iD: 0000-0003-1816-1315
SPIN 代码: 6810-3279
MD, Cand. Sci. (Med)
俄罗斯联邦, MoscowRoman V. Reshetnikov
Moscow Center for Diagnostics and Telemedicine
Email: reshetnikov@fbb.msu.ru
ORCID iD: 0000-0002-9661-0254
SPIN 代码: 8592-0558
Cand. Sci. (Phys.-Math.)
俄罗斯联邦, MoscowViktor Yu. Bosin
Moscow Center for Diagnostics and Telemedicine
Email: bosin@npcmr.ru
ORCID iD: 0000-0002-4619-2744
SPIN 代码: 3380-7889
MD, Dr. Sci. (Med.)
俄罗斯联邦, MoscowOlga V. Omelyanskaya
Moscow Center for Diagnostics and Telemedicine
Email: o.omelyanskaya@npcmr.ru
ORCID iD: 0000-0002-0245-4431
SPIN 代码: 8948-6152
俄罗斯联邦, Moscow
Anton V. Vladzymyrskyy
Moscow Center for Diagnostics and Telemedicine; The First Sechenov Moscow State Medical University (Sechenov University)
Email: a.vladzimirskiy@npcmr.ru
ORCID iD: 0000-0002-2990-7736
SPIN 代码: 3602-7120
MD, Dr. Sci (Med.)
俄罗斯联邦, Moscow; Moscow参考
- De Koning HJ, van der Aalst CM, de Jong PA, et al. Reduced lung-cancer mortality with volume CT screening in a randomized trial. N Engl J Med. 2020;382(6):503–513. doi: 10.1056/NEJMoa1911793
- Henschke CI, Boffetta P, Yankelevitz DF, Altorki N. Computed tomography screening: The International Early Lung Cancer Action Program Experience. Thoracic Sur Clin. 2015;25(2):129–143. doi: 10.1016/j.thorsurg.2014.12.001
- Callister ME, Baldwin DR, Akram AR, et al. Correction: British Thoracic Society guidelines for the investigation and management of pulmonary nodules: Accredited by NICE. Thorax. 2015;70(Suppl 2):ii1–ii54. doi: 10.1136/thoraxjnl-2015-207168
- Oudkerk M, Devaraj A, Vliegenthart R, et al. European Position Statement on Lung Cancer Screening. Lancet Oncology. 2017;18(12):e754–766. doi: 10.1016/S1470-2045(17)30861-6
- Wood DE, Kazerooni EA, Baum SL, et al. Lung cancer screening, version 3.2018, NCCN clinical practice guidelines in oncology. J Natl Compr Canc Netw. 2018;16(4):412–441. doi: 10.6004/jnccn.2018.0020
- Horeweg N, Scholten ET, de Jong PA, et al. Detection of lung cancer through low-dose CT screening (NELSON): A prespecified analysis of screening test performance and interval cancers. Lancet Oncology. 2014;15(3):1342–1350. doi: 10.1016/S1470-2045(14)70387-0
- Oudkerk M, Liu S, Heuvelmans MA, et al. Lung cancer LDCT screening and mortality reduction: Evidence, pitfalls and future perspectives. Nat Rev Clin Oncol. 2021;18(3):135–151. doi: 10.1038/s41571-020-00432-6
- Duffy SW, Field JK. Mortality reduction with low-dose CT screening for lung cancer. N Engl J Med. 2020;382(6):572–573. doi: 10.1056/NEJMe1916361
- Morozov SP, Kuzmina ES, Vetsheva NN, et al. Moscow screening: Screening of lung cancer using low-dose computed tomography. Problems Social Hygiene Healthcare History Med. 2019;27(S):630–636. (In Russ). doi: 10.32687/0869-866X-2019-27-si1-630-636
- Gombolevsky VA, Barchuk AA, Laipan AS, et al. Lung сancer screening with low-dose computed tomography: Management and efficiency. Radiology Practice. 2018;(1):28–36. (In Russ).
- Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33(1):159–174.
- Revel MP, Bissery A, Bienvenu M, et al. Are two-dimensional ct measurements of small noncalcified pulmonary nodules reliable? Radiology. 2004;231(2):453–458. doi: 10.1148/radiol.2312030167
- Xie X, Willemink MJ, Zhao Y, et al. Inter- and intrascanner variability of pulmonary nodule volumetry on low-dose 64-row CT: an anthropomorphic phantom study. BJR. 2013;86(1029):20130160. doi: 10.1259/bjr.20130160
- Kulberg NS, Reshetnikov RV, Novik VP, et al. Inter-observer variability between readers of CT images: all for one and one for all. Digital Diagnostics. (In Russ). 2021;2(2):105–118 doi: 10.17816/DD60622
补充文件