Diagnostic accuracy of artificial intelligence for the screening of prostate cancer in biparametric magnetic resonance imaging: a systematic review
- Authors: Kryuchkova O.V.1, Schepkina E.V.2,3,4, Rubtsova N.A.5, Alekseev B.Y.5, Kuznetsov A.I.6, Epifanova S.V.1,3, Zarya E.V.1, Talyshinskii A.E.7
-
Affiliations:
- Central Clinical Hospital, Office of the President of the Russian Federation
- Russian Presidential Academy of National Economy and Public Administration
- Research and Practical Clinical Center for Diagnostics and Telemedical Technologies
- Editorial of the Journal “Pediatria” named after G.N. Speransky
- P.A. Herzen Moscow Oncology Research Institute, Branch National Medical Research Radiological Center
- Moscow Aviation Institute
- Saint Petersburg State University
- Issue: Vol 5, No 3 (2024)
- Pages: 534-550
- Section: Systematic reviews
- URL: https://journals.rcsi.science/DD/article/view/310036
- DOI: https://doi.org/10.17816/DD626643
- ID: 310036
Cite item
Full Text
Abstract
BACKGROUND: Based on the latest published data, 40,137 new cases of prostate cancer were reported in Russia in 2021, ranking second after lung cancer in men.
Thus, prostate cancer is one of the most common malignant neoplasms in men. Accurate and timely detection of prostate cancer is important under the current conditions.
AIM: This systematic review aimed to assess the quality of prediction models designed to detect prostate cancer during initial presentation.
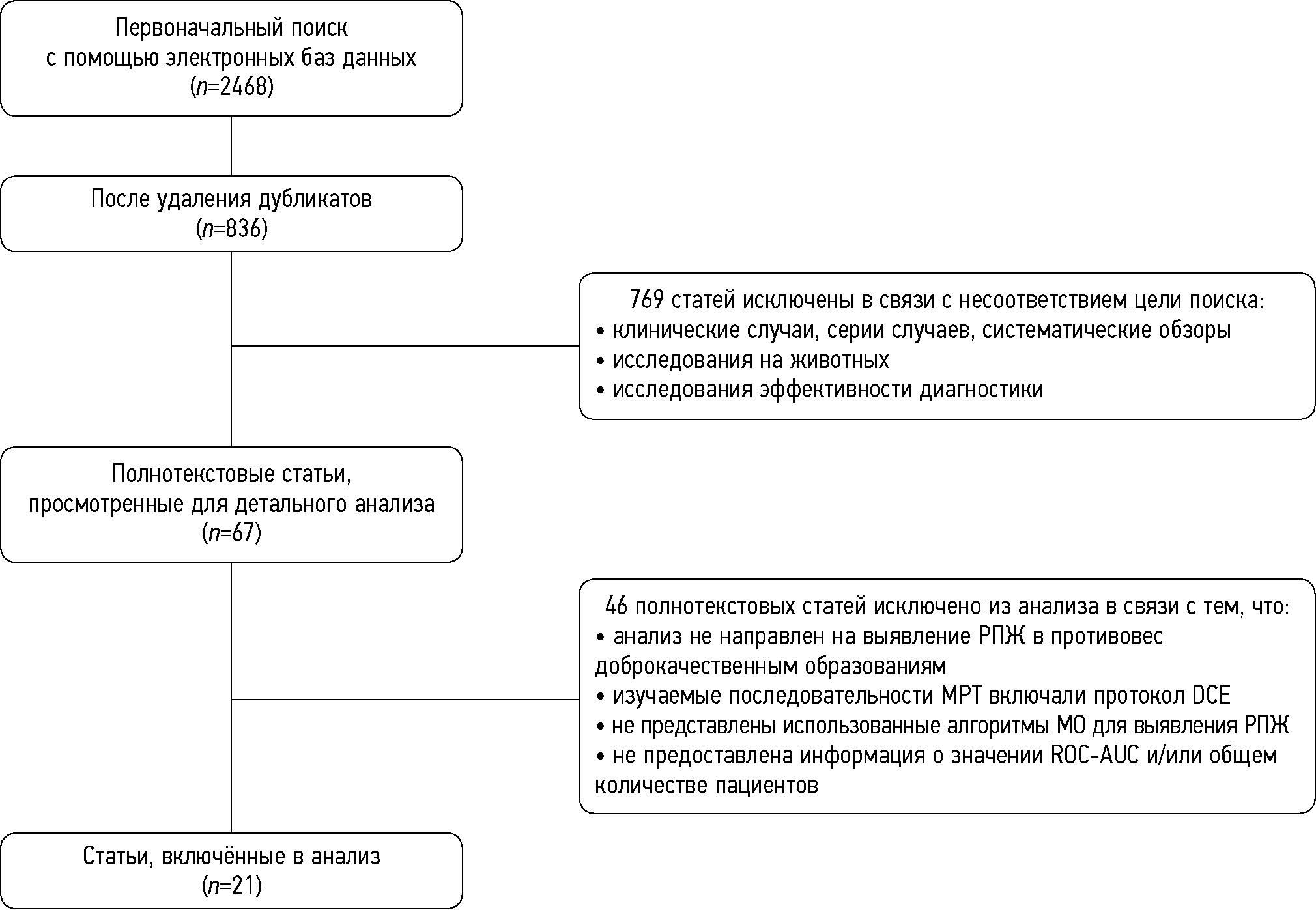
MATERIALS AND METHODS: A systematic search was performed in eLibrary.ru, PubMed, Google Scholar, Web of Science, and ResearchGate for relevant publications indexed from January 2019 to September 2023 in accordance with the PRISMA protocol. Two authors independently assessed the relevant studies for potential inclusion or exclusion.
RESULTS: This systematic review meta-analysis included 21 studies. In total, data from 3,630 patients were analyzed, of which 47% had prostate cancer and 53% had benign prostate neoplasms. The mean age of the patients was 67.1 (36–90) years. In addition, 81% of the studies were based on T2-weighted imaging, 57% on diffusion-weighted imaging, and 76% on apparent diffusion coefficient. Moreover, 43% and 33% of the studies were dedicated to transition zone and prostate peripheral zone neoplasms, respectively, and 52% of the authors examined the whole prostate gland, without dividing it into zones. The most common machine-learning algorithms applied by the investigators were as follows: multiple logistic regression (76%), support vector machine (38%), and random forest (24%). Based on the meta-analysis performed for the receiver operating characteristic-area under the curve (ROC–AUC) assessment with random-effect approach in 73 prediction models described in the publications, the final ROC–AUC was 0.793 [95% CI 0.768–0.818], I2 = 86.71%, p <0.001. The most accurate prediction models were based on the T2-weighted imaging + apparent diffusion coefficients imaging protocol: 0.860 [95% CI 0.813–0.907], and models created according to the “white box” principle (0.834 [95% CI 0.806–0.861]) were more accurate than the “black box” ones (0.733 [95% CI 0.695–0.771]). The models using radiomics and clinical features were slightly more accurate than those using the radiomics parameters alone (0.869 [95% CI 0.844–0.895] vs. 0.779 [95% CI 0.751–0.807]). Model accuracy was nearly identical across transitional and/or peripheral zone studies.
CONCLUSIONS: Artificial intelligence demonstrated promising results. However, the clinical applicability may require more intensive expert inspection in healthcare institutions and evaluation of efficacy in prospective studies.
Full Text
##article.viewOnOriginalSite##About the authors
Oksana V. Kryuchkova
Central Clinical Hospital, Office of the President of the Russian Federation
Email: ovk16@bk.ru
ORCID iD: 0000-0001-6483-2074
SPIN-code: 2445-3370
MD Cand. Sci. (Medicine)
Russian Federation, MoscowElena V. Schepkina
Russian Presidential Academy of National Economy and Public Administration; Research and Practical Clinical Center for Diagnostics and Telemedical Technologies; Editorial of the Journal “Pediatria” named after G.N. Speransky
Author for correspondence.
Email: elenaschepkina@gmail.com
ORCID iD: 0000-0002-2079-1482
SPIN-code: 2347-9436
Scopus Author ID: 57211515165
ResearcherId: IAR-4060-2023
Cand. Sci. (Sociology)
Russian Federation, Moscow; Moscow; MoscowNatalia A. Rubtsova
P.A. Herzen Moscow Oncology Research Institute, Branch National Medical Research Radiological Center
Email: rna17@ya.ru
ORCID iD: 0000-0001-8378-4338
SPIN-code: 9712-9091
MD, Dr. Sci. (Medicine)
Russian Federation, MoscowBoris Y. Alekseev
P.A. Herzen Moscow Oncology Research Institute, Branch National Medical Research Radiological Center
Email: byalekseev@mail.ru
ORCID iD: 0000-0002-3398-4128
SPIN-code: 4692-5705
MD, Dr. Sci. (Medicine)
Russian Federation, MoscowAnton I. Kuznetsov
Moscow Aviation Institute
Email: drednout5786@yandex.ru
ORCID iD: 0000-0003-2182-5792
SPIN-code: 8824-9080
Russian Federation, Moscow
Svetlana V. Epifanova
Central Clinical Hospital, Office of the President of the Russian Federation; Research and Practical Clinical Center for Diagnostics and Telemedical Technologies
Email: svepifanova@yandex.ru
ORCID iD: 0000-0002-7591-5120
SPIN-code: 9067-5033
MD, Cand. Sci. (Medicine)
Russian Federation, Moscow; MoscowElena V. Zarya
Central Clinical Hospital, Office of the President of the Russian Federation
Email: zaryya@yandex.ru
ORCID iD: 0009-0001-4444-8881
SPIN-code: 9800-8219
Russian Federation, Moscow
Ali E. Talyshinskii
Saint Petersburg State University
Email: ali-ma@mail.ru
ORCID iD: 0000-0002-3521-8937
SPIN-code: 7747-0117
MD, Dr. Sci. (Medicine)
Russian Federation, Saint PetersburgReferences
- Mottet N, van den Bergh RCN, Briers E, et al. EAU-EANM-ESTRO-ESUR-SIOG Guidelines on Prostate Cancer–2020 Update. Part 1: Screening, Diagnosis, and Local Treatment with Curative Intent. European urology. 2021;79(2):243–262. doi: 10.1016/j.eururo.2020.09.042
- Zdravookhranenie v Rossii, 2021: statisticheskii sbornik. Moscow: Rosstat; 2021.
- Verma S, Rajesh A. A Clinically Relevant Approach to Imaging Prostate Cancer: review. American Journal of Roentgenology. 2011;196(3 Suppl):S1–10 Quiz S11–4. doi: 10.2214/AJR.09.7196
- Girometti R, Giannarini G, Panebianco V, et al. Comparison of different thresholds of PSA density for risk stratification of PI-RADSv2.1 categories on prostate MRI. The British Journal of Radiology. 2022;95(1131):20210886. doi: 10.1259/bjr.20210886
- Niaf E, Lartizien C, Bratan F, et al. Prostate Focal Peripheral Zone Lesions: Characterization at Multiparametric MR Imaging–Influence of a Computer-aided Diagnosis System. Radiology. 2014;271(3):761–769. doi: 10.1148/radiol.14130448
- Drost FJH, Osses DF, Nieboer D, et al. Prostate MRI, with or without MRI-targeted biopsy, and systematic biopsy for detecting prostate cancer. Cochrane Database of Systematic Reviews. 2019;4(4):CD012663. doi: 10.1002/14651858.CD012663.pub2
- Goldenberg SL, Nir G, Salcudean SE. A new era: artificial intelligence and machine learning in prostate cancer. Nature Reviews Urology. 2019;16(7):391–403. doi: 10.1038/s41585-019-0193-3
- Cuocolo R, Cipullo MB, Stanzione A, et al. Machine learning applications in prostate cancer magnetic resonance imaging. European Radiology Experimental. 2019;3(1):35. doi: 10.1186/s41747-019-0109-2
- Ghezzo S, Bezzi C, Presotto L, et al. State of the art of radiomic analysis in the clinical management of prostate cancer: A systematic review. Critical Reviews in Oncology/Hematology. 2022;169:103544. doi: 10.1016/j.critrevonc.2021.103544
- Gelezhe PB, Blokhin IA, Semenov SS, Caruso D. Magnetic resonance imaging radiomics in prostate cancer radiology: what is currently known? Digital Diagnostics. 2021;2(4):441–452. doi: 10.17816/DD70170
- Ferro M, de Cobelli O, Vartolomei MD, et al. Prostate Cancer Radiogenomics–From Imaging to Molecular Characterization. International Journal of Molecular Sciences. 2021;22(18):9971. doi: 10.3390/ijms22189971
- Steyerberg EW, Vickers AJ, Cook NR, et al. Assessing the Performance of Prediction Models. Epidemiology. 2010;21(1):128–138. doi: 10.1097/EDE.0b013e3181c30fb2
- Higgins JPT, Green S, editors. The Cochrane Collaboration. Cochrane Handbook for Systematic Reviews of Interventions [Internet]. England: John Wiley & Sons Ltd. [cited 19 Mar 2020]. Available from: https://training.cochrane.org/handbook
- Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–560. doi: 10.1136/bmj.327.7414.557
- DerSimonian R, Laird N. Meta-analysis in clinical trials. Controlled Clinical Trials. 1986;7(3):177–188. doi: 10.1016/0197-2456(86)90046-2
- Woźnicki P, Westhoff N, Huber T, et al. Multiparametric MRI for Prostate Cancer Characterization: Combined Use of Radiomics Model with PI-RADS and Clinical Parameters. Cancers (Basel). 2020;12(7):1767. doi: 10.3390/cancers12071767
- Li M, Yang L, Yue Y, et al. Use of Radiomics to Improve Diagnostic Performance of PI-RADS v2.1 in Prostate Cancer. Frontiers in Oncology. 2021;10:631831. doi: 10.3389/fonc.2020.631831
- Gui S, Lan M, Wang C, et al. Application Value of Radiomic Nomogram in the Differential Diagnosis of Prostate Cancer and Hyperplasia. Frontiers in Oncology. 2022;12:859625. doi: 10.3389/fonc.2022.859625
- Lu Y, Li B, Huang H, et al. Biparametric MRI-based radiomics classifiers for the detection of prostate cancer in patients with PSA serum levels of 4~10 ng/mL. Frontiers in Oncology. 2022;12:1020317. doi: 10.3389/fonc.2022.1020317
- Zhou B, Liu X, Gan H, et al. Differentiation of Prostate Cancer and Stromal Hyperplasia in the Transition Zone With Monoexponential, Stretched-Exponential Diffusion-Weighted Imaging and Diffusion Kurtosis Imaging in a Reduced Number of b Values: Correlation With Whole-Mount Pathology. Journal of Computer Assisted Tomography. 2022;46(4):545–550. doi: 10.1097/RCT.0000000000001314
- Wu M, Krishna S, Thornhill RE, et al. Transition zone prostate cancer: Logistic regression and machine-learning models of quantitative ADC, shape and texture features are highly accurate for diagnosis. Journal of Magnetic Resonance Imaging. 2019;50(3):940–950. doi: 10.1002/jmri.26674
- Zhong JG, Shi L, Liu J, et al. Predicting prostate cancer in men with PSA levels of 4–10 ng/mL: MRI-based radiomics can help junior radiologists improve the diagnostic performance // Scientific reports. 2023;13(1):4846. doi: 10.1038/s41598-023-31869-1
- Ou YC, Chang KH, Tung MC, et al. Building a Nomogram for Prediction of Prostate Cancer in Patients With Preoperatively Suspected Prostate Cancer. Anticancer Research. 2020;40(5):2995–3002. doi: 10.21873/anticanres.14280
- McGarry SD, Bukowy JD, Iczkowski KA, et al. Gleason Probability Maps: A Radiomics Tool for Mapping Prostate Cancer Likelihood in MRI Space. Tomography. 2019;5(1):127–134. doi: 10.18383/j.tom.2018.00033
- Hu L, Zhou DW, Fu CX, et al. Advanced zoomed diffusion-weighted imaging vs. full-field-of-view diffusion-weighted imaging in prostate cancer detection: a radiomic features study. European radiology. 2021;31(3):1760–1769. doi: 10.1007/s00330-020-07227-4
- Ji X, Zhang J, Shi W, et al. Bi-parametric magnetic resonance imaging based radiomics for the identification of benign and malignant prostate lesions: cross-vendor validation. Physical and Engineering Sciences in Medicine. 2021;44(3):745–754. doi: 10.1007/s13246-021-01022-1
- Jin P, Shen J, Yang L, et al. Machine learning-based radiomics model to predict benign and malignant PI-RADS v2.1 category 3 lesions: a retrospective multi-center study. BMC Medical Imaging. 2023;23(1):47. doi: 10.1186/s12880-023-01002-9
- Li S, Zheng T, Fan Z, et al. A dynamic-static combination model based on radiomics features for prostate cancer using multiparametric MRI. Physics in Medicine & Biology. 2023;68(1):015008. doi: 10.1088/1361-6560/aca954
- Ayyad SM, Badawy MA, Shehata M, et al. A New Framework for Precise Identification of Prostatic Adenocarcinoma. Sensors. 2022;22(5):1848. doi: 10.3390/s22051848
- Han L, He G, Mei Y, et al. Combining Magnetic Resonance Diffusion-Weighted Imaging with Prostate-Specific Antigen to Differentiate Between Malignant and Benign Prostate Lesions. Medical Science Monitor. 2022;28:e935307. doi: 10.12659/MSM.935307
- Chen T, Li M, Gu Y, et al. Prostate Cancer Differentiation and Aggressiveness: Assessment With a Radiomic-Based Model vs. PI-RADS v2. Journal of Magnetic Resonance Imaging. 2019;49(3):875–884. doi: 10.1002/jmri.26243
- He D, Wang X, Fu C, et al. MRI-based radiomics models to assess prostate cancer, extracapsular extension and positive surgical margins. Cancer Imaging. 2021;21(1):46. doi: 10.1186/s40644-021-00414-6
- Jamshidi G, Abbasian Ardakani A, Ghafoori M, et al. Radiomics-based machine-learning method to diagnose prostate cancer using mp-MRI: a comparison between conventional and fused models. Magnetic Resonance Materials in Physics, Biology and Medicine. 2022;36(1):55–64. doi: 10.1007/s10334-022-01037-z
- Aussavavirojekul P, Hoonlor A, Srinualnad S. Optimization of clinical risk-factor interpretation and radiological findings with machine learning for PIRADS category 3 patients. Prostate. 2022;82(2):235–244. doi: 10.1002/pros.24266
- Giambelluca D, Cannella R, Vernuccio F, et al. PI-RADS 3 Lesions: Role of Prostate MRI Texture Analysis in the Identification of Prostate Cancer. Current Problems in Diagnostic Radiology. 2021;50(2):175–185. doi: 10.1067/j.cpradiol.2019.10.009
- Viswanath SE, Chirra PV, Yim MC, et al. Comparing radiomic classifiers and classifier ensembles for detection of peripheral zone prostate tumors on T2-weighted MRI: a multi-site study. BMC Medical Imaging. 2019;19(1):22. doi: 10.1186/s12880-019-0308-6
- Chawla NV, Bowyer KW, Hall LO, Kegelmeyer WP. SMOTE: Synthetic Minority Over-sampling Technique. Journal of Artificial Intelligence Research. 2002;16(1):321–357.
- Dai JC, Morgan TN, Goueli R, et al. MRI Features Associated with Histology of Benign Prostatic Hyperplasia Nodules: Generation of a Predictive Model. Journal of Endourology. 2022;36(3):381–386. doi: 10.1089/end.2021.0397
- Liu J, Dong B, Qu W, et al. Using clinical parameters to predict prostate cancer and reduce the unnecessary biopsy among patients with PSA in the gray zone. Scientific reports. 2020;10(1):5157. doi: 10.1038/s41598-020-62015-w
- Zhang L, Tang M, Chen S, et al. A meta-analysis of use of Prostate Imaging Reporting and Data System Version 2 (PI-RADS V2) with multiparametric MR imaging for the detection of prostate cancer. European radiology. 2017;27(12):5204–5214. doi: 10.1007/s00330-017-4843-7
- Zhen L, Liu X, Yegang C, et al. Accuracy of multiparametric magnetic resonance imaging for diagnosing prostate Cancer: a systematic review and meta-analysis. BMC Cancer. 2019;19(1):1244. doi: 10.1186/s12885-019-6434-2
Supplementary files