Creation of a training and test dataset with the disposition and transposition of overlaying electrocardiographic electrodes when recording electrocardiograms-12
- Authors: Gazashvili T.M.1, Drozdov D.V.2, Shutov D.V.3, Shkoda A.S.1
-
Affiliations:
- City Clinical Hospital No. 67 named after L.A. Vorokhobov
- National Medical Research Centre of Cardiology Named After Academician E.I. Chazov
- Research and Practical Clinical Center for Diagnostics and Telemedicine Technologies
- Issue: Vol 4, No 2 (2023)
- Pages: 133-141
- Section: Datasets
- URL: https://journals.rcsi.science/DD/article/view/146881
- DOI: https://doi.org/10.17816/DD201870
- ID: 146881
Cite item
Abstract
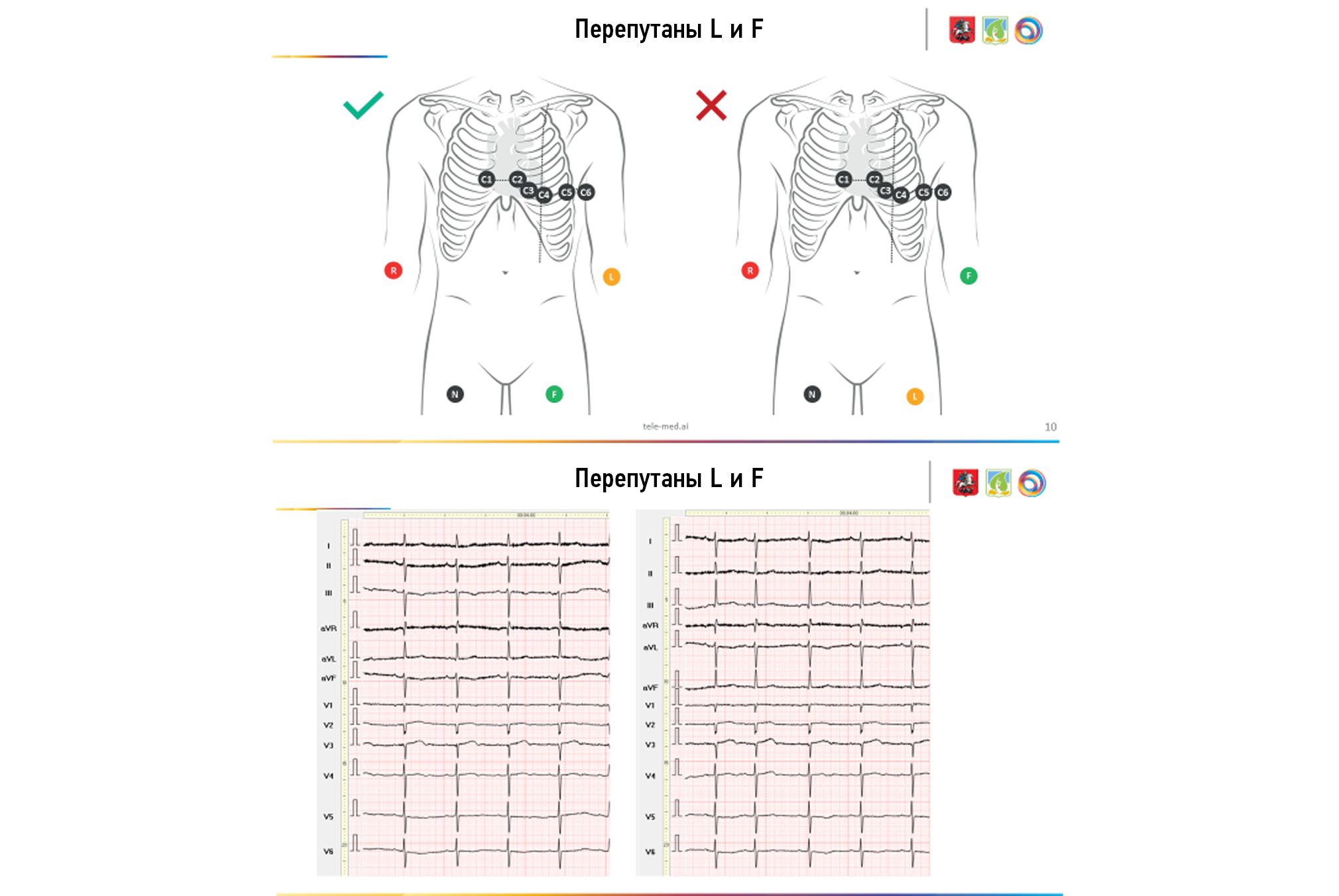
BACKGROUND: Electrocardiography is one of the simplest, most widely used, inexpensive, and informative methods in functional diagnostics; yet, if performed poorly, its diagnostic value is sharply reduced. Several attempts were made to systematize errors and deviations in electrode application, but all concerned the most common options (rearrangement of red and yellow electrodes, yellow and green electrodes, and chest electrodes — above or below the standard scheme).
AIM: To create an electrocardiogram dataset with different options for transpositions and dispositions of electrodes during electrocardiogram recording.
MATERIALS AND METHODS: The study included patients aged 18–75 years (27 males and 22 females). All patients provided informed consent for electrocardiogram registration. During one visit, the cardiogram was recorded on the device “Modular system for recording and remote transmission of electrocardiograms (EASY ECG)” for each patient.
RESULTS: In all, 488 electrocardiograms were recorded in 49 patients. The results obtained indicate a significant variability of the electrocardiogram pattern. Visual analysis of the electrocardiograms revealed no difficulties in determining the transposition associated with rearranging the leads on the arms (RY) in the thoracic C1–C2. The placement of thoracic electrodes in contact cheek-to-cheek dispositions with the transfer of thoracic leads above or below two intercostals was reliably determined compared with the Wilson scheme. The transpositions of the yellow and green limb electrodes and the change in the position of the thoracic ones when they are “lined up” in a straight line, “bullied” between the ribs (curved), and confused in places C5 and C6 are difficult to determine even when comparing two cardiograms next to each other, with the correct and transpositional superposition of the electrodes. The initial changes on the electrocardiograms, physique type, breast size, or the presence of an implant most likely determine it.
CONCLUSION: An electrocardiography dataset was obtained using various electrode dislocation variants. The dataset consists of a series of electrocardiograms obtained for each patient with several electrode placement options and contains both normal and pathological electrocardiograms.
Full Text
##article.viewOnOriginalSite##About the authors
Tamara M. Gazashvili
City Clinical Hospital No. 67 named after L.A. Vorokhobov
Email: Tamaradoc24@gmail.com
ORCID iD: 0000-0002-5875-9699
SPIN-code: 4208-2303
Russian Federation, Moscow
Dmitry V. Drozdov
National Medical Research Centre of Cardiology Named After Academician E.I. Chazov
Email: cardioexp@gmail.com
ORCID iD: 0000-0001-7374-3604
SPIN-code: 2279-9657
MD, Cand. Sci. (Med)
Russian Federation, MoscowDmitry V. Shutov
Research and Practical Clinical Center for Diagnostics and Telemedicine Technologies
Email: ShutovDV@zdrav.mos.ru
ORCID iD: 0000-0003-1836-3689
SPIN-code: 9381-2456
MD, Dr. Sci. (Med)
Russian Federation, MoscowAndrey S. Shkoda
City Clinical Hospital No. 67 named after L.A. Vorokhobov
Author for correspondence.
Email: a.shkoda@67gkb.ru
ORCID iD: 0000-0002-9783-1796
SPIN-code: 4520-2141
MD, Dr. Sci. (Med)
Russian Federation, MoscowReferences
- Rosen AV, Koppikar S, Shaw C, Baranchuk A. Common ECG lead placement errors. Part I: Limb lead reversals. Int J Med Students. 2014;2(3):92–98. doi: 10.5195/ijms.2014.95
- Rosen AV, Koppikar S, Shaw C, Baranchuk A. Common ECG lead placement errors. Part II: precordial misplacements. Int J Med Students. 2014;2(3):99–103. doi: 10.5195/ijms.2014.96
- Jekova I, Krasteva V, Leberet R, et al. Inter-lead correlation analysis for automated detection of cable reversals in 12/16-lead ECG. Comput Methods Programs Biomed. 2016;(134):31–41. doi: 10.1016/j.cmpb.2016.06.003
- Kania M, Rix H, Fereniec M, et al. The effect of precordial lead displacement on ECG morphology. Med Biological Engineering Computing. 2014;52(2):109–119. doi: 10.1007/s11517-013-1115-9.
- Wenger W, Kligfield P. Variability of precordial electrode placement during routine electrocardiography. J Electrocardiol. 1996;29(3):179–184. doi: 10.1016/s0022-0736(96)80080-x
- García-Niebla J, Llontop-García P, Valle-Racero JI, et al. Technical mistakes during the acquisition of the electrocardiogram. Ann Noninvasive Electrocardiol. 2009;14(4):389–403. doi: 10.1111/j.1542-474X.2009.00328.x
- Peberdy MA, Ornato JP. Recognition of electrocardiographic lead misplacements. Am J Emergency Med. 1993;11(4):403–405. doi: 10.1016/0735-6757(93)90177-d
- Kemp B, Olivan J. European data format ‘plus’ (EDF+), an EDF alike standard format for the exchange of physiological data. Clin Neurophysiol. 2003;114(9):1755–1761. doi: 10.1016/s1388-2457(03)00123-8
- Drozdov DV, Shutov DV, Gazashvili TM, et al. Coordination of medical ECG descriptions using a thesaurus (list of standard phrases) of conclusions. Medical Alphabet. 2022;(10):19–26. (In Russ). doi: 10.33667/2078-5631-2022-11-19-26
Supplementary files