The importance of the role of T-cell immunity in the development of modern tick-borne encephalitis vaccines
- Authors: Tigeeva E.V.1, Nizolenko L.F.1, Karpenko L.I.1
-
Affiliations:
- State Research Center of Virology and Biotechnology “Vector”
- Issue: Vol 101, No 4 (2024)
- Pages: 546-559
- Section: REVIEWS
- URL: https://journals.rcsi.science/0372-9311/article/view/264253
- DOI: https://doi.org/10.36233/0372-9311-553
- EDN: https://elibrary.ru/icslhy
- ID: 264253
Cite item
Abstract
The tick-borne encephalitis (TBE) virus is highly pathogenic and can affect the central nervous system, leading to severe chronic effects or death. The only effective measure to combat TBE is vaccine prophylaxis. Vaccines that are currently used for mass immunization are based on inactivated TBE virus, they provide a protective immune response, but such vaccines require multiple administrations. A possible reason for short-term immunity is an incomplete functional T-cell response to these types of vaccines.
The aim of this review is to analyze the literature on the role of the T-cell immune response in protecting the body from tick-borne encephalitis, its importance for vaccine development, and to consider approaches to the development of new TBE vaccines based on different platforms.
When preparing the review, we analyzed the literature presented in scientific databases — PubMed, Scopus, Elsevier, Google Scholar as of April 2024. The following keywords were used for the search: vaccine, tick-borne encephalitis virus, T-cell immune response, flaviviruses.
A several publications have demonstrated that T-cell responses following natural infection with TBE virus and after vaccination with inactivated virus are different. During viral infection, both Th1- and Th2-type CD4+ T cells and CD8+ T cells are activated and play an important role in the elimination of viral infection. After vaccination, the only Th2-type CD4+ T-cell response predominates, which may be the reason for the short-lived immune response.
To date, a number of different types of experimental TBE vaccines are being studied, such as live-attenuated vaccines, viral vector vaccines, subunit vaccines, virus-like particles, DNA and mRNA vaccines, and polyepitope immunogens. In our opinion, the most promising in terms of T-cell response activation are vaccines based on T-cell polyepitope immunogens delivered in the form of DNA or mRNA.
Full Text
The wide spread of the tick-borne encephalitis (TBE) virus is a serious concern for public health authorities in many countries. This is due to the fact that the virus, being highly pathogenic, can affect the central nervous system (CNS), leading to severe chronic consequences or death [1–3].
In 30% of cases, neurological complications develop in people who have contracted TBE. Mortality from infection varies depending on the strain of the virus. The highest percentage of fatal cases (up to 35%) is registered when infected with strains belonging to the Far Eastern subtype [4–6].
Vaccine prophylaxis is the most effective way to control the virus. All currently licensed vaccines are based on inactivated strains of TBE. It is considered that the average seroconversion rate for both Russian and European vaccines ranges between 86–100%, which ensures the formation of protective immunity in vaccinated individuals [2, 7]. At the same time, vaccines based on inactivated TBE virus have a number of disadvantages: complicated vaccination schedule, relatively high reactogenicity, complexity of production and storage; in addition, there are cases of breakthrough infections in vaccinated persons [2, 8, 9]. Among vaccinated persons, the incidence of TBE ranges from 3.7% [10] to 23.8% [11] of the total number of cases, depending on the endemic region. One possible reason for breakthrough infections is the lack of vaccines that take into account the genetic variability of the TBE virus. Another reason is due to insufficiently intense and short-lived specific immunity in a number of vaccinated individuals, especially the elderly [7–9, 12].
The T-cell immune response is an important part of protective immunity against viral infections such as TBE. There are an increasing number of publications on the role of the T-cell immune response in the defense against infection with TBE virus. Therefore, more and more researchers have begun to pay attention to this aspect of the adaptive immune response, especially in the context of studies devoted to the development of new vaccine preparations [7, 13]. The wide spread of the virus and the significant growth of the number of patients have stimulated interest in the development of new vaccines against TBE virus, taking into account the role of the T-cell immune response.
The aim of the review is to analyze the literature on the role of the T-cell immune response in protecting the body from tick-borne encephalitis, its importance for vaccine development, and to consider approaches to the development of new TBE vaccines based on different platforms.
In this review, we consider the main aspects of T-cell response formation in humans when infected with TBE virus and after vaccination with licensed vaccines, as well as the main directions of work on the search for safe and highly effective next-generation vaccines that can overcome the limitations of the existing ones.
Materials and methods
The following keywords were used for the search: vaccines, tick-borne encephalitis virus, T-cell immune response, flaviviruses.
In the first phase, a search using different combinations of keywords in the scientific electronic database PubMed retrieved 1754 sources. Restricting the search to the time of publication from 2019 to 2024 allowed us to narrow the search to 424 sources. A search without considering the year of publication in this research library found an additional 123 sources matching the subject matter. Similarly, the search was conducted using the scientific databases Scopus, Elsevier, Google Scholar.
During the literature search in these databases in Russian and English languages, which was carried out taking into account such selection criteria as year of publication and accessibility of publications to reading, about 2000 sources corresponding to the topic were analyzed. Due to article length limitations, 88 sources were selected.
Adaptive immune response during infection with TBE virus and after vaccination
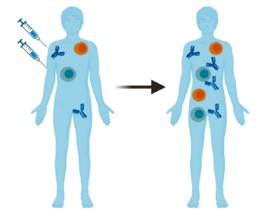
The adaptive immune response consists of humoral (antibody-mediated) and cellular immune responses specific to the TBE virus. The figure schematically represents the immune reactions of the adaptive immune response occurring after vaccination or during infection with TBE virus
Иммунные реакции, возникающие после заражения вирусом КЭ (А) и после вакцинации против КЭ (Б) (по R. Ackermann-Gäumann и соавт. [13]).
Immune reactions occurring after infection with the TBE virus and after vaccination against TBE (adapted from R. Ackermann-Gäumann et al. [13]).
The efficacy of antibodies against the TBE virus has been demonstrated by protecting susceptible individuals exposed to the virus by administering them anti-TBEV-immunoglobulin. Humoral immunity is thought to play a crucial role in defense against the TBE virus by providing synthesis of antibodies specifically targeting the virus. These antibodies neutralize the virus and prevent its spread, helping to limit the severity of infection and providing long-term immunity against infection with the TBE virus (Figure, A). Antibodies are able to bind to viral particles, causing them to be engulfed and destroyed by phagocytic immune cells [7, 13].
Memory B cells and virus-neutralizing antibodies are formed in a person who has had TBE, which provide long-term protection against virus re-infection. The long-term maintenance of memory B cells allows the immune system to respond more quickly and effectively to re-infection. When the same virus is encountered again, these cells rapidly differentiate into plasma cells that produce antibodies that destroy the virus before it can cause widespread infection and disease [13–16].
When vaccinated with inactivated virus, the functionality of memory B-cell populations is relatively short-lived due to limited CD4+ T-cell responses (Figure, B) [17].
Immune response associated with CD4+ T cells
CD4+ T lymphocytes are important in the formation of both humoral and cellular immunity. CD4+ T-cells are important producers of cytokines that help stimulate the antiviral immune response and provide B cells with the assistance needed to stimulate antibody synthesis (Figure, A). TBE virus encodes 7 non-structural proteins (NS1, NS2a, NS2b, NS3, NS4a, NS4b and NS5) and only 3 structural proteins: protein C (capsid) and the membrane-associated proteins prM/M (membrane/membrane precursor) and E (envelope) [18-20]. The structural proteins appear to contain the major epitopes that activate the CD4+ T cell response during infection [8, 21], although there is evidence in the literature that several T helper epitopes are contained in the non-structural protein of the TBE virus, NS1 [22].
When analyzing peptide fragments of protein C predicted immunodominant epitopes, it was shown that mainly two peptide clusters are involved in CD4+-cell activation both in natural disease and after vaccination. They are located in the α2- and α4-helixes of protein C [21]. The clusters of epitopes predicted for E protein were less effective with respect to CD4+ activation, but this difference cannot be considered significant. It was found that in patients who underwent natural infection, specific stimulation of CD4+ cells is provided by epitopes located in the 3rd domain, as well as in the stem region of the E-protein. In the group of vaccinated patients, stimulation was provided by peptide clusters from the 1st, 2nd and 3rd domains of the E-protein [21].
TBE virus-specific CD4+ T-cells generated by vaccination appear to respond to a narrower range of viral targets than those generated by infection [8, 21], with vaccine-induced levels of interferon-γ (IFN-γ) reaching only about half the level of response induced by infection.
It is noteworthy that after natural infection with TBE virus, naive CD4+ cells differentiate predominantly along the Th1 pathway, while during vaccination with inactivated virus — to a greater extent along the Th2 pathway [8, 9]. At the same time, against the background of natural infection, CD4+ T cells acquire polyfunctionality, producing various cytokines, such as interleukin-2 (IL-2), IFN-γ and tumor necrosis factor-α (TNF-α; Figure, A) [4]. There is a correlation between the functionality of CD4+ T-cells and the level of virus-neutralizing antibodies, indicating that they are able to control the induction of neutralizing antibodies [8].
After vaccination, the number of CD4+ T-cells also positively correlates with the antibody response against TBE virus [17], and vaccine responders show increased proliferation of antigen-specific T-cells compared to non-responders (Figure, A) [23]. The response to vaccination tends to be skewed towards IL-2 and TNF-α production compared to infection (Figure, B) [9].
Immune response associated with CD8+ T cells
CD8+ T lymphocytes play an important role in viral infection by identifying and destroying infected cells, thereby limiting the spread of the virus in the body. To date, unlike CD4+ T cells, CD8+ T-lymphocyte-specific epitopes have only been found in non-structural proteins of the TBE virus, such as NS2A, NS3, NS4B and NS5 [24].
CD8+ T-cells are activated somewhat later than CD4+ T cells during natural infection, but nevertheless have a significantly higher level of activation, producing increased levels of granzyme B and perforin [4, 7]
K. Blom et al. showed that in patients with TBE at the peak of the T-cell response one week after hospitalization, CD8+ T-cell activation was significantly increased compared to CD4+ T-cells [25], indicating a tendency towards CD8+ dominance (Figure, A). These CD8+ T cells additionally exhibited an effector phenotype (CD45RA-CCR7) [24, 25] and had a highly activated Eomes+Ki67+T-bet+ transcriptional profile. However, these effectors tended to be monofunctional. After acute infection, when patients recovered, antigen-specific CD8+ T cells switched to the Eomes-Ki67-T-bet+ phenotype [25], which corresponds to a type 1 effector memory population.
Usually, CD8+ T-cell analysis is performed in patients with a severe course of the disease, in whom CD8+ T-cells are not only found in the blood, but sometimes also in brain tissue [13]. This fact limits the understanding of whether the CD8+ population is an important protective factor in mild or asymptomatic disease or an additional factor causing pathology [13]. In favor of the necessity of CD8+ T-cells for the body's defense against the TBE virus is the recent evidence that the severity of the disease, as well as its form, depends on the degree of T cell activation. Early activation of T-cell responses, including a subset of CD8+ T-lymphocytes, significantly correlated with a favorable outcome of the disease [26].
The results of animal studies are also mixed. The study by D. Růzek et al. showed that mice with severe immunodeficiency and mice with CD8 knockout had a higher survival rate after lethal infection caused by TBE virus compared to wild-type mice or mice with adoptively transferred CD8+ T-cells [27]. This may suggest a possible role of CD8+ T cells in the development of lethal infection. Thereafter D. Růzek et al. obtained data indicating that CD8+ T-cells are not responsible for the permeability of the blood-brain barrier during the disease, since its destruction during infection caused by this virus was observed both in wild-type and CD8 knockout animals [28].
The role of CD8+ T cells in virus clearance from neural tissues has been shown for other flavivirus infections using mice as laboratory animals [29]. Depletion of CD8+ T cells leads to enhanced infection by Zika and dengue viruses, but this effect is reversed after adoptive transfer of memory CD8+ T cells. Similar conclusions were obtained using mice deficient in various cytotoxic effector molecules in West Nile fever virus. During the initial stages of infections caused by yellow fever and Zika viruses, when mice has not yet formed a sufficient levels of virus-specific antibodies, effector CD8+ T cells are essential for infection control [29].
There are few data on the presence of specific CD8+ T cells in humans who have received the TBE vaccine (Figure, B). A. Sycheva et al. analyzed the formation of T-cell response in volunteers vaccinated with Tick-E-Vac and showed that in the peripheral blood of the vaccinated individuals a low level of CD8+ specific to the TBE virus was detected, and the overall response to the vaccine clearly depends on CD4+ [30, 31].
As mentioned above, the main epitopes of CD8+ T-cells are contained in nonstructural proteins of the virus [24]. Since non-structural proteins are synthesized only during active virus replication, such proteins are found in small amounts or are completely absent in currently used vaccines based on inactivated virus [32]. This fact may partially explain the low CD8+ T-cell response during vaccination. That said, TBE infection can induce a lifelong protective CD8+ response [14].
A number of vaccine platforms will be discussed below in terms of the possibility of inducing a T-cell immune response.
Vaccines against tick-borne encephalitis virus
Vaccines based on inactivated virus
There are currently a number of approved and licensed adult and pediatric TBE vaccines based on inactivated strains of the virus [33]. In Europe, two vaccines based on European strains of TBE virus are available: K23 and Neudorfl. In Russia, the Tick-E-Vac vaccine and its lyophilized analogue called TBE vaccine Moscow (FSBSI“Chumakov FSC R&D IBP RAS”) and EnceVir (Microgen), created on the basis of the Far Eastern strains of the TBE virus, Sofyin and 205, respectively, are licensed [12, 34–36]. The vaccine used in China is based on the Sen-Zhang strain (Far Eastern subtype of TBE virus) [37]. Vaccination against TBE virus has proven to be effective, as evidenced by the results of mass vaccination campaigns in Austria [38] and Russia [39–42].
All licensed vaccines are capable of providing sufficiently effective prevention of TBE, especially when large-scale vaccination programs are implemented. However, the existing vaccines are not without disadvantages, including a complicated vaccination schedule due to the inability to maintain an adequate level of immune protection in the long term. Failure to adhere to a patient's vaccination schedule can lead to low levels of humoral immune response in the vaccinated, especially in the elderly [2, 7].
Vaccination with inactivated virus provides lower levels of antibodies than with natural infection [7]. It is suggested that this may be due to a change in the conformation of the E-protein as a result of the effect exposure of formaldehyde on the viral particle during the inactivation process. Thus, the availability of epitopes that bind to neutralizing antibodies is reduced [43]. As already mentioned, there is a difference in the immune response to infection and vaccination with inactivated virus, which is associated with the limited T-cell responses — a small number of specific CD8+ T-lymphocytes, as well as reduced functionality of CD4+ cells (Figure, B). In response to inactivated virus, mono- or bi-functional CD4+ T cells are formed, capable of producing, for example, IL-2 alone or IL-2 and TNF-α alone, but the level of IFN-γ secretion is significantly reduced compared to natural infection [4, 8]. Vaccination leads to a shift of the response towards the Th2-pathway, whereas in natural disease, the cellular response is usually formed along the Th1-pathway, which may affect the efficacy of protection against the virus [7, 44]. Ideally, vaccines should elicit more robust responses of IFN-γ-producing CD4+ T-cells.
The disadvantages of vaccines based on inactivated viruses include the fact that they are produced using only a specific strain of TBE virus and do not take into account its genetic variability. As a result, in endemic regions, the number of breakthrough infections among vaccinated individuals can reach 23.8% of the total number of cases [11]. Despite this, the direction of creating inactivated vaccines remains paramount. In 2017, phase I/II clinical trials of the Evervac vaccine were completed. The main difference of this vaccine from its analogs is the absence of adjuvants in its composition, as well as virus production in Vero cells, which allows for an improved safety profile. However, the problem of incomplete T-cell response has not been solved yet [45].
Approaches to TBE vaccine development and induction of cell-mediated immunity
To date, research on candidate vaccines against TBE virus and other flaviviruses has focused on several objectives at once:
- achieve high immunogenicity in all age and risk groups;
- ensure rapid and high levels of seroconversion;
- ensure the development of a long-term immune response by avoiding complex immunization regimens;
- reduce side effects;
- provide cross-protective immunity against several subtypes of TBE virus and induction of an effective CD4+- and CD8+-cell response [7].
In addition to the widely used approach of creating TBE vaccines based on inactivated virus, various experimental prophylactic vaccines based on different platforms are currently being developed [7].
Live attenuated vaccines
Live attenuated viruses that have lost their pathogenic properties at the genetic level, but contain the same antigens as the original pathogen and retain the ability to cause natural infection in the body in a weakened form, contribute to the formation of a pronounced and long-lasting B- and T-cell immunity, which is close to post-infection immunity in terms of intensity [46]. The first attempts to attenuate the TBE virus were not successful. Therefore, the Langat TR-21 virus, discovered in 1956 [7, 19], was considered as a more promising source of strains for live attenuated vaccines against TBE virus. However, a large study involving 650,000 volunteers showed that, in addition to induction of a high level of immune protection, the development of serious neurological consequences, including encephalitis, was often observed among those vaccinated with attenuated Langat virus [7]. Subsequent studies on the development of live-attenuated TBE vaccines have continued to improve their safety profile. Proteins such as C, E and NS5 were selected as the main targets for phenotype attenuation, which eventually led to several candidate vaccines with low reactogenicity and high levels of antibody production and T-cell response [47–49].
Work is actively underway to produce chimeric viruses combining fragments of the genomes of the TBE virus, most often the genes of the E and prM proteins, as well as West Nile, dengue, and Langat viruses [7, 50].
Although vaccines based on live attenuated viruses raise serious safety concerns, several vaccines have already been licensed worldwide against infections caused by other flaviviruses: yellow fever (YFV-17D), Japanese encephalitis (IMOJEV), and dengue fever (Dengvaxia). Two quadrivalent live attenuated dengue fever vaccines produced by Takeda Pharmaceutical and NIH/Butantan have successfully completed Phase III clinical trials [50].
Subunit vaccines
Compared to live attenuated vaccines, the production and use of subunit vaccines is characterized by safety due to the possibility of including individual antigenic components in the form of viral proteins or their fragments in the vaccine. However, subunit vaccines induce mainly only a humoral immune response and a limited range of T-cell responses. They are unable to induce a prolonged immune response and therefore require the inclusion of adjuvants and booster immunizations.
Many potential vaccines being developed against TBE virus and infections caused by other flaviviruses have been based on structural protein E or its subunits containing epitopes recognized by neutralizing antibodies [7]. It was shown that immunization of mice with recombinant EDIII-domain of protein E in combination with various adjuvants allows to achieve not only induction of neutralizing antibodies, but also partial protection from virus infection [51]. Subunit vaccines against Dengue fever (V180) and West Nile fever (WN-80E), which contain truncated forms of protein E with adjuvants, have shown significant success in clinical trials [50].
Virus-like particles
Virus-like particles (VLPs) are formed as a result of simultaneous synthesis of structural proteins, most often prM/E, in different expression systems. The structure of VLPs is close to the native structure of the TBE virion, which allows the maximum number of T- and B-cell epitopes to be presented to immunocompetent cells. Such vaccines are characterized by the absence of potential pathogenic properties and a high level of safety [50]. VLPs administration is accompanied by the induction of a high titer of virus-neutralizing antibodies, activation of CD4+ T-cells, and formation of central and effector memory T cells [7]. In one of the studies on the immunogenic properties of VLPs in a mouse model, it was shown that VLPs immunization promotes differentiation of CD4+ T-cells along the Th2-pathway with a predominance of IL-4+ phenotype [52]. A similar study indirectly confirmed this result. After VLPs administration to mice, a robust humoral immune response was observed; however, analysis of CD4+ T-cells for IFN-γ, IL-2, and TNF-α showed no significant difference between experimental and control groups [53].
Vaccines based on viral vectors
Vaccines against TBE virus and diseases caused by related viruses are also being developed using an approach that has proven effective against other infections — viral vector-based vaccines. Such vaccines are recombinant or modified viruses encoding specific antigens and characterized by the ability or inability to replicate after introduction into the body. The main advantage of vaccines based on viral vectors is their high immunogenicity due to the intracellular expression of antigens and the presence of the viral vector itself, which can play the role of a natural adjuvant [50].
However, as with live attenuated vaccines, viral vector-based approaches, especially those capable of replication, raise questions about the safety of their use due to the increased risks of high viremia and the potential for acquisition of pathogenic properties. When viral vector-based vaccines are administered, an anti-vector immune response is formed, which reduces the efficacy of the vaccines in re-immunization. The disadvantages of such vaccines should also include complexity and costliness of their production [50].
Vectors based on such viruses as recombinant influenza A virus, recombinant adenovirus, modified Vaccinia virus, etc. are used in works on the development of experimental vaccines against flavivirus infections. [7]. Various combinations of TBE virus antigens, which are encoded in the genome of the viral carrier, make it possible to modulate the immune response if necessary. Thus, a number of studies have shown that various viral vectors encoding NS1 sequences induce the synthesis of virus-neutralizing antibodies and also provide partial protection against TBE virus [54]. At the same time, such vaccines can also activate the T-cell mediated immunity by inducing the formation of IFN-γ, IL-2 and TNF-α producing CD4+- and CD8+-T-lymphocytes.. A modified Vaccinia virus Ankara encoding the TBE virus prM and E protein sequence, when administered to mice, also induced high levels of virus-neutralizing antibodies and specific T-cell response, and provided complete protection against virus infection [55]. Similar results were obtained in a study investigating the properties of a candidate vaccine against Zika fever based on recombinant vesicular stomatitis virus encoding prM, E and NS1 proteins [56].
Despite the effectiveness of using viral vectors as a platform for vaccine development, only one vaccine has reached the clinical trial stage to date. MV-ZIKV against Zika fever has been developed on the platform of the Schwarz strain of measles virus and is in Phase I clinical trials [57].
mRNA and DNA vaccines
Recently, nucleic acid-based platforms, such as DNA- and mRNA-based vaccines, have been actively developed. The intracellular expression of antigens encoded by nucleic acid-based vaccines allows for the native structure of proteins due to posttranslational modifications [58]. This is important for further processing of the antigen, its presentation on the surface of immune cells, and activation of both CD4+- and CD8+ T cells.
The technology of production of such vaccines does not require complex manipulations or work with dangerous pathogens, which greatly facilitates the process of their creation and reduces its overall cost [58]. Furthermore, the use of such vaccines is believed to be safer compared to traditional approaches [59].
However, it should be noted that nucleic acid-based vaccines in their naked form have low immunogenicity; therefore, various delivery methods to immunocompetent cells, both chemical and physical, are used to improve their efficacy [50].
Several studies on obtaining experimental vaccines against TBE virus based on nucleic acids have been published. An experimental vaccine was obtained based on self-replicating non-infectious RNA of TBE virus containing several deletions in the C-protein gene region and point mutations in the prM gene region, but without loss of replicative function. The resulting mRNA vaccine effectively induced not only humoral but also cellular response, activating CD8+ cells as well as the response of Th1-type CD4+ T cells [60–62].
DNA vaccines have an advantage over mRNA vaccines due to their greater stability and less demanding storage conditions. The works of Y. Omori-Urabe et al. [63] and a group of researchers from University of Vienna (Austria) [64] described DNA constructs in the form of plasmid and viral vectors encoding E and prM proteins. Immunization with these constructs induced a strong immune response and a high level of virus-neutralizing antibodies. As a rule, the Th1 pathway of CD4+-cell differentiation accompanied by the production of IFN-γ, TNF-α and IL-2 was observed during the administration of such vaccines; however, some variability in the shift of the Th1/Th2 ratio was demonstrated depending on the use of certain delivery methods [64].
Several experimental mRNA and DNA vaccines against other flavivirus infections (caused by dengue, Zika, and West Nile viruses) are also currently in clinical trials, and many others are being considered in preclinical studies [50].
Polyepitope vaccines
This vaccine platform specializes in the design of specifically T-cell immunogens and relies on two main strategies. The first polyepitope strategy is based on the design of artificial genes, delivered either by plasmid DNA or mRNA, or by a viral vector, encoding chains of CD4+ and CD8+ epitopes of various virus proteins, linked by linkers, lined up into a single artificial vaccine construct. This strategy gives the investigator the freedom to choose epitopes, which provides a narrower focus of responses on preferred epitopes [65]. Current knowledge of the mechanisms of CD4+- and CD8+-response formation to a productive viral infection allows us to develop algorithms for optimal selection of T-cell epitopes of the target pathogen, taking into account the peculiarities of the major histocompatibility complex (MHC) of a particular genotype. Currently, there are epitope databases such as the Immune Epitope Database [66], programs have been developed to predict T-cell epitopes in various viral proteins, and programs for rational vaccine design, such as PolyCTLDesigner [67].
The second strategy is to construct chimeric immunogens created from longer stretches of proteins covering the most conserved regions of viral proteins where T-cell epitopes are concentrated [65]. Bioinformatic approaches that are used in optimizing epitope compounds for polyepitope vaccines are also used in the design of conserved chimeric polyepitope proteins.
In the last three years, hundreds of papers have been published on the design of polyepitope immunogens for flaviviruses (Zika [68], dengue [69], Powassan [70, 71], and yellow fever [72] viruses), as well as SARS-CoV-2 [73–77], Ebola virus [78–80], Marburg virus [81], influenza [82–85], and others. The immunogenicity of polyepitope HIV-1 vaccines has been evaluated in clinical trials [86, 87].
D.N. Kisakov et al. described an experimental DNA TBE vaccine encoding an artificial polyepitope immunogen of the TBE virus [88]. The immunogen included predicted epitopes from the major proteins of the TBE virus (NS1, NS3, NS5, and E) restricted by the most common human allomorphs of HLA type I molecules and allelic variants of MHC type I molecules characteristic of BALB/c mice. Administration of this vaccine induces the formation of a protective virus-specific T-cell response in mice and provides 50% protection of immunised animals against infection with 100 LD50 of TBE virus (strain 205) [88].
Immunogens designed using computerized methods of T-cell epitope prediction and rational design of polyepitope antigens can become the basis for new effective methods of immunoprophylaxis of infectious diseases. They can be used to design both “universal” antigenic constructs covering a significant part of the target human population and personalized constructs tailored to the genetic features of a particular patient (taking into account his/her repertoire of allelic variants of class I and/or II MHC molecules).
With regard to vaccines against TBE virus the optimal way to improve vaccine efficacy may be an integrated strategy that combines the use of two immunogens in a prime-boost system, one of which induces virus-neutralizing antibodies (e.g., traditional inactivated vaccine) and the other induces T-cell responses (polyepitope immunogen).
Conclusion
With the accumulation of data on the peculiarities of the adaptive immune response in TBE, the role of the T-cell response in protective immunity during infection and vaccination, as well as its influence on the outcome of the disease, is becoming clearer. T-cell responses following natural infection with TBE virus and after vaccination with inactivated virus are different. During viral infection, both Th1- and Th2-type CD4+ T cells and CD8+ T cells are activated and play an important role in the elimination of viral infection. The absence of non-structural proteins of the TBE virus carrying the main epitopes of CD8+ T-lymphocytes in the composition of inactivated vaccines leads to the activation of only a part of the T-cell immune response represented by CD4+ T-cells of Th2-type, which mainly provide support for the B-cell response. Thus, the incompleteness of the T-cell immune response occurring after vaccination with classical vaccines leads to reduced functionality of memory cells, which may underlie the short duration of the protective response to the vaccine.
Several questions regarding the T-cell response remain unclear, including the role of CD8+ in the development of the pathologic process during infection. Nevertheless, many researchers conclude that a high level of virus-neutralizing antibodies combined with a T-cell response, including the response of specific CD8+ T-cells, is a prerequisite for limiting the entry of TBE into CNS organs and mitigating immune pathology.
Attention to the T-cell response continues to grow also due to the need to improve classical inactivated vaccines against TBE virus. Research into next-generation vaccines is focused on finding a strategy that provides a balanced humoral and T-cell immune response. To date, a number of different types of experimental TBE vaccines are being studied, such as live-attenuated vaccines, viral vector vaccines, subunit vaccines, virus-like particles, DNA and mRNA vaccines, and polyepitope immunogens. In our opinion, the most promising in terms of T-cell response activation are vaccines based on T-cell polyepitope immunogens delivered in the form of DNA or mRNA. The optimal way to improve vaccine efficacy may be an integrated strategy that combines the use of two immunogens in a prime-boost system, one of which induces virus-neutralizing antibodies and the other induces T-cell responses.
The development of a safe, effective TBE vaccine that provides balanced T- and B-cell immunity will be a major advance in the fight against TBE virus.
About the authors
Elena V. Tigeeva
State Research Center of Virology and Biotechnology “Vector”
Author for correspondence.
Email: tigeeva_ev@vector.nsc.ru
ORCID iD: 0009-0001-5203-2130
junior researcher, Bioengineering department
Russian Federation, KoltsovoLily F. Nizolenko
State Research Center of Virology and Biotechnology “Vector”
Email: tigeeva_ev@vector.nsc.ru
ORCID iD: 0000-0002-9647-4969
Cand. Sci. (Biol.), senior researcher, Bioengineering department
Russian Federation, KoltsovoLarisa I. Karpenko
State Research Center of Virology and Biotechnology “Vector”
Email: tigeeva_ev@vector.nsc.ru
ORCID iD: 0000-0003-4365-8809
D. Sci. (Biol.), Head, Laboratory of recombinant vaccines, leading researcher, Bioengineering department
Russian Federation, KoltsovoReferences
- Хаснатинов M.A. Роль генетического разнообразия вируса клещевого энцефалита и других клещевых патогенов в обеспечении устойчивого существования их эпидемиологически значимых природных очагов в Восточной Сибири и Монголии: Дисс. … д-ра биол. наук. Иркутск;2019. Khasnatinov M.A. The role of the genetic diversity of tick-borne encephalitis virus and other tick-borne pathogens in ensuring the sustainable existence of their epidemiologically significant natural foci in Eastern Siberia and Mongolia: Diss. Irkutsk;2019.
- Колясникова Н.М., Ишмухаметов А.А., Акимкин В.Г. Современное состояние проблемы клещевого энцефалита в России и мире. Эпидемиология и вакцинопрофилактика. 2023;22(1):104–23. Kolyasnikova N.M., Ishmukhametov A.A., Akimkin V.G. The current state of the problem of tick-borne encephalitis in Russia and the world. Epidemiology and Vaccinal Prevention. 2023;22(1):104–23. DOI: https://doi.org/10.31631/2073-3046-2023-22-1-104-123 EDN: https://elibrary.ru/yeynhd
- Колясникова Н.М., Герасимов С.Г., Ишмухаметов А.А., Погодина В.В. Эволюция клещевого энцефалита за 80-летний период: основные проявления, вероятные причины. Эпидемиология и вакцинопрофилактика. 2020;19(3):78–88. Kolyasnikova N.M., Gerasimov S.G., Ishmukhametov A.A., Pogodina V.V. Evolution of tick-borne encephalitis over an 80-year period: main manifestations, probable causes. Epidemiology and Vaccinal Prevention. 2020;19(3):78–88. DOI: https://doi.org/10.31631/2073-3046-2020-19-3-78-88 EDN: https://elibrary.ru/kihhki
- Blom K., Cuapio A., Sandberg J.T., et al. Cell-mediated immune responses and immunopathogenesis of human tick-borne encephalitis virus-infection. Front. Immunol. 2018;9:2174. DOI: https://doi.org/10.3389/fimmu.2018.02174
- Bogovic P., Lotric-Furlan S., Strle F. What tick-borne encephalitis may look like: clinical signs and symptoms. Travel Med. Infect. Dis. 2010;8(4):246–50. DOI: https://doi.org/10.1016/j.tmaid.2010.05.011
- Bogovic P., Strle F. Tick-borne encephalitis: A review of epidemiology, clinical characteristics, and management. World J. Clin. Cases. 2015;3(5):430–41. DOI: https://doi.org/10.12998/wjcc.v3.i5.430
- Kubinski M., Beicht J., Gerlach T., et al. Tick-borne encephalitis virus: a quest for better vaccines against a virus on the rise. Vaccines (Basel). 2020;8(3):451. DOI: https://doi.org/10.3390/vaccines8030451
- Aberle J.H., Schwaiger J., Aberle S.W., et al. Human CD4 + T helper cell responses after tick-borne encephalitis vaccination and infection. PLoS One. 2015;10(10):e0140545. DOI: https://doi.org/10.1371/journal.pone.0140545
- Varnaitė R., Blom K., Lampen M.H., et al. Magnitude and functional profile of the human CD4+ T cell response throughout primary immunization with tick-borne encephalitis virus vaccine. J. Immunol. 2020;204(4):914–22. DOI: https://doi.org/10.4049/jimmunol.1901115
- Лучинина С.В., Семенов А.И., Степанова О.Н. и др. Вакцинопрофилактика клещевого энцефалита в Челябинской области: масштабы вакцинации, популяционный иммунитет, анализ случаев заболевания привитых. Эпидемиология и вакцинопрофилактика. 2016;15(1):67–76. Luchinina S.V., Semenov A.I., Stepanova O.N., et al. Vaccinal prevention of tick-borne encephalitis in Chelyabinsk region: dynamics of vaccination, population immunity, analysis of TBE cases in vaccinated persons. Epidemiology and Vaccinal Prevention. 2016;15(1):67–76. DOI: https://doi.org/10.31631/2073-3046-2016-15-1-67-76 EDN: https://elibrary.ru/vldhlb
- Погодина В.В., Щербинина М.C., Скрынник С.М. и др. Эпидемиологическая ситуация по клещевому энцефалиту и вакцинопрофилактика в Курганской области (1983–2017 гг.). Эпидемиология и вакцинопрофилактика. 2018;17(4):46–55. Pogodina V.V., Shcherbinina M.S., Skrynnik S.M., et al. Epidemiological situation of tick-borne encephalitis in the Kurgan region (1983–2017). Epidemiology and Vaccinal Prevention. 2018;17(4):46–55. DOI: https://doi.org/10.31631/2073-3046-2018-17-4-46-56 EDN: https://elibrary.ru/xxfrcx
- Козлова Т.Ю., Хантимирова Л.М., Рукавишников А.В., Шевцов В.А. Анализ эффективности и безопасности вакцин для профилактики клещевого энцефалита. БИОпрепараты. Профилактика, диагностика, лечение. 2018;18(1):33–41. Kozlova T.Yu., Khantimirova L.M., Rukavishnikov A.V., Shevtsov V.A. Analysis of efficacy and safety of tick-borne encephalitis vaccines. Biological Products. Prevention, Diagnosis, Treatment. 2018;18(1):33–41. DOI: https://doi.org/10.30895/2221-996X-2018-18-1-33-41
- Ackermann-Gäumann R., Lang P., Zens K.D. Defining the "Correlate(s) of Protection" to tick-borne encephalitis vaccination and infection – key points and outstanding questions. Front. Immunol. 2024;15:1352720. DOI: https://doi.org/10.3389/fimmu.2024.1352720
- Remoli M.E., Marchi A., Fortuna C., et al. Anti-tick-borne encephalitis (TBE) virus neutralizing antibodies dynamics in natural infections versus vaccination. Pathog. Dis. 2015;73(2):1–3. DOI: https://doi.org/10.1093/femspd/ftu002
- Dörrbecker B., Dobler G., Spiegel M., Hufert F.T. Tick-borne encephalitis virus and the immune response of the mammalian host. Travel Med. Infect. Dis. 2010;8(4):213–22. DOI: https://doi.org/10.1016/j.tmaid.2010.05.010
- Worku D.A. Tick-Borne Encephalitis (TBE): From tick to pathology. J. Clin. Med. 2023;12(21):6859. DOI: https://doi.org/10.3390/jcm12216859
- Aberle J.H., Stiasny K., Kundi M., Heinz F.X. Mechanistic insights into the impairment of memory B cells and antibody production in the elderly. Age (Dordr.). 2013;35(2):371–81. DOI: https://doi.org/10.1007/s11357-011-9371-9
- Lindquist L., Vapalahti O. Tick-borne encephalitis. Lancet. 2008;371(9627):1861–71. DOI: https://doi.org/10.1016/S0140-6736(08)60800-4
- Gritsun T.S., Lashkevich V.A., Gould E.A. Tick-borne encephalitis. Antiviral. Res. 2003;57(1-2):129–46. DOI: https://doi.org/10.1016/s0166-3542(02)00206-1
- Simmonds P., Becher P., Bukh J., et al. ICTV virus taxonomy profile: flaviviridae. J. Gen. Virol. 2017;98(1):2–3. DOI: https://doi.org/10.1099/jgv.0.000672
- Schwaiger J., Aberle J.H., Stiasny K., et al. Specificities of human CD4+ T cell responses to an inactivated flavivirus vaccine and infection: correlation with structure and epitope prediction. J. Virol. 2014;88(14):7828–42. DOI: https://doi.org/10.1128/JVI.00196-14
- Волкова Т.Д., Короев Д.О., Титова М.А. и др. Синтетические фрагменты белка ns1 вируса клещевого энцефалита, обладающие протективным действием. Биоорганическая химия. 2007;33(2):213–7. Volkova T.D., Koroev D.O., Titova M.A., et al. Synthetic fragments of the NS1 protein of the tick-borne encephalitis virus exhibiting a protective effect. Russian Journal of Bioorganic Chemistry. 2007;33(2):213–7. DOI: https://doi.org/10.1134/S1068162007020021 EDN: https://elibrary.ru/lkjlvr
- Garner-Spitzer E., Wagner A., Paulke-Korinek M., et al. Tick-borne encephalitis (TBE) and hepatitis B nonresponders feature different immunologic mechanisms in response to TBE and influenza vaccination with involvement of regulatory T and B cells and IL-10. J. Immunol. 2013;191(5):2426–36. DOI: https://doi.org/10.4049/jimmunol.1300293
- Lampen M.H., Uchtenhagen H., Blom K., et al. Breadth and dynamics of HLA-A2- and HLA-B7-Restricted CD8+ T cell responses against nonstructural viral proteins in acute human tick-borne encephalitis virus infection. Immunohorizons. 2018;2(6):172-84. DOI: https://doi.org/10.4049/immunohorizons.1800029
- Blom K., Braun M., Pakalniene J., et al. Specificity and dynamics of effector and memory CD8 T cell responses in human tick-borne encephalitis virus infection. PloS Pathog. 2015; 11(1):e1004622. DOI: https://doi.org/10.1371/journal.ppat.1004622
- Aregay A., Slunečko J., Bogovic P., et al. Poor virus-specific T-cell responses early after tick-borne encephalitis virus infection correlate with disease severity. Emerg. Microbes Infect. 2024;13(1):2317909. DOI: https://doi.org/10.1080/22221751.2024.2317909
- Růzek D., Salát J., Palus M., et al. CD8+ T-cells mediate immunopathology in tick-borne encephalitis. Virology. 2009;384(1):1–6. DOI: https://doi.org/10.1016/j.virol.2008.11.023
- Růžek D., Salát J., Singh S.K., Kopecký J. Breakdown of the blood-brain barrier during tick-borne encephalitis in mice is not dependent on CD8+ T-cells. PloS One. 2011;6(5):e20472. DOI: https://doi.org/10.1371/journal.pone.0020472
- Slon Campos J.L., Mongkolsapaya J., Screaton G.R. The immune response against flaviviruses. Nat. Immunol. 2018;19(11):1189–98. DOI: https://doi.org/10.1038/s41590-018-0210-3
- Sycheva A., Komech E., Pogorelyy M., et al. Inactivated tick-borne encephalitis vaccine elicits several overlapping waves of T cell response. Front. Immunol. 2022;13:970285. DOI: https://doi.org/10.3389/fimmu.2022.970285
- Gomez I., Marx F., Saurwein-Teissl M., et al. Characterization of tick-borne encephalitis virus-specific human T lymphocyte responses by stimulation with structural TBEV proteins expressed in a recombinant baculovirus. Viral Immunol. 2003;16(3):407–14. DOI: https://doi.org/10.1089/088282403322396190
- Salat J., Mikulasek K., Larralde O., et al. Tick-borne encephalitis virus vaccines contain non-structural protein 1 antigen and may elicit NS1-specific antibody responses in vaccinated individuals. Vaccines (Basel). 2020;8(1):81. DOI: https://doi.org/10.3390/vaccines8010081
- Hansson K.E., Rosdahl A., Insulander M., et al. Tick-borne encephalitis vaccine failures: a 10-year retrospective study supporting the rationale for adding an extra priming dose in individuals starting at age 50 years. Clin. Infect. Dis. 2020;70(2):245–51. DOI: https://doi.org/10.1093/cid/ciz176
- Šmit R., Postma M.J. Review of tick-borne encephalitis and vaccines: clinical and economical aspects. Expert Rev. Vaccines. 2015;14(5):737–47. DOI: https://doi.org/10.1586/14760584.2015.985661
- Воробьева М.С., Эльберт Л.Б., Грачев В.П. и др. Реактогенность и иммунологическая эффективность концентрированной очищенной вакцины против клещевого энцефалита. Вопросы вирусологии. 1983;28(5):622–6. Vorob'eva M.S., El'bert L.B., Grachev V.P., et al. Reactogenicity and immunological effectiveness of a concentrated, purified vaccine against tick-borne encephalitis. Problems of Virology. 1983;28(5):622–6.
- Ворович М.Ф., Майкова Г.Б., Чернохаева Л.Л. и др. Иммунологическая эффективность и безопасность вакцины «Клещ-Э-вак»: «взрослая» форма. Вопросы вирусологии. 2017;62(2):73–80. Vorovitch M.F., Maikova G.B., Chernokhaeva L.L., et al. Immunogenicity and safety of the adult TBE vaccine «Tick-E-Vac». Problems of Virology. 2017; 62(2):73–80. DOI: https://doi.org/10.18821/0507-4088-2017-62-2-73-80 EDN: https://elibrary.ru/yjkhft
- Yoshii K., Song J.Y., Park S.B., et al. Tick-borne encephalitis in Japan, Republic of Korea and China. Emerg. Microbes Infect. 2017;6(9):e82. DOI: https://doi.org/10.1038/emi.2017.69.
- Heinz F.X., Stiasny K., Holzmann H., et al. Vaccination and tick-borne encephalitis, central Europe. Emerg. Infect. Dis. 2013; 19(1):69–76. DOI: https://doi.org/10.3201/eid1901.120458
- Пеньевская Н.А., Рудаков Н.В., Рудакова С.А. Проблемные аспекты оценки эпидемиологической эффективности вакцинопрофилактики клещевого энцефалита. Эпидемиология и вакцинопрофилактика. 2018;17(5):78–88. Penyevskaya N.A., Rudakov N.V., Rudakova S.A. Problematic aspects of the evaluation of the epidemiological effectiveness of vaccination against tick-borne encephalitis. Epidemiology and Vaccinal Prevention. 2018;17(5):78–88. DOI: https://doi.org/10.31631/2073-3046-2018-17-5-78-88 EDN: https://elibrary.ru/yqxvdv
- Романенко В.В., Есюнина М.С., Килячина А.С., Пименова Т.А. Массовая иммунизация населения Свердловской области против клещевого энцефалита, ее эпидемиологическая, клиническая и иммунологическая эффективность вакцинопрофилактики. Медицинская вирусология. 2006;23:116–25. Romanenko V.V., Esyunina M.S., Kilyachina A.S., Pimenova T.A. Mass immunization Sverdlovsk region population against tickborne encephalitis, its epidemiological, clinical and immunological effectiveness of vaccination. Medical Virology. 2006;23:116–25.
- Романенко В.В., Есюнина М.С., Килячина А.С. Опыт реализации программы массовой иммунизации населения против клещевого энцефалита в Свердловской области. Вопросы вирусологии. 2007;52(6):22–5. Romanenko V.V., Yesyunina M.S., Kilyachina A.S. Experience in implementing the mass immunization program against tick-borne encephalitis in the Sverdlovsk Region. Problems of Virology. 2007;52(6):22–5. EDN: https://elibrary.ru/icdgcd
- Щербинина М.С., Бархалева О.А., Дорохова О.С., Мовсесянц А.А. Эффективность специфической профилактики клещевого энцефалита. БИОпрепараты. Профилактика, диагностика, лечение. 2020;20(3):174–86. Shcherbinina M.S., Barkhaleva O.A., Afonina O.S., Movsesyants A.A. Effectiveness of specific prevention of tick-borne encephalitis. Biological Products. Prevention, Diagnosis, Treatment. DOI: https://doi.org/10.30895/2221-996X-2020-20-3-174-186 EDN: https://elibrary.ru/xjyyhs
- Kuivanen S., Hepojoki J., Vene S., et al. Identification of linear human B-cell epitopes of tick-borne encephalitis virus. Virol. J. 2014;11:115. DOI: https://doi.org/10.1186/1743-422X-11-115
- Morozova O.V., Bakhvalova V.N., Potapova O.F., et al. Evaluation of immune response and protective effect of four vaccines against the tick-borne encephalitis virus. Vaccine. 2014;32(25):3101–6. DOI: https://doi.org/10.1016/j.vaccine.2014.02.046
- Vorovitch M.F., Grishina K.G., Volok V.P., et al. Evervac: phase I/II study of immunogenicity and safety of a new adjuvant-free TBE vaccine cultivated in Vero cell culture. Hum. Vaccin. Immunother. 2020;16(9):2123–30. DOI: https://doi.org/10.1080/21645515.2020.1757990
- Алпатова Н.А., Авдеева Ж.И., Гайдерова Л.А. и др. Иммунный ответ при иммунизации противовирусными вакцинами. БИОпрепараты. Профилактика, диагностика, лечение. 2020;20(1):21–9. Alpatova N.A., Avdeeva Zh.I., Gayderova L.A., et al. Immune response induced by immunisation with antiviral vaccines. Biological Products. Prevention, Diagnosis, Treatment. 2020;20(1):21–9. DOI: https://doi.org/10.30895/2221-996X-2020-20-1-21-29 EDN: https://elibrary.ru/tbqndr
- de Fabritus L., Nougairède A., Aubry F., et al. Attenuation of tick-borne encephalitis virus using large-scale random codon re-encoding. PLoS Pathog. 2015;11(3):e1004738. DOI: https://doi.org/10.1371/journal.ppat.1004738
- Kofler R.M., Heinz F.X., Mandl C.W. Capsid protein C of tick-borne encephalitis virus tolerates large internal deletions and is a favorable target for attenuation of virulence. J. Virol. 2002;76(7):3534–43. DOI: https://doi.org/10.1128/jvi.76.7.3534-3543.2002
- Mandl C.W., Allison S.L., Holzmann H., et al. Attenuation of tick-borne encephalitis virus by structure-based site-specific mutagenesis of a putative flavivirus receptor binding site. J. Virol. 2000;74(20):9601–9. DOI: https://doi.org/10.1128/jvi.74.20.9601-9609.2000
- Dutta S.K., Langenburg T. A perspective on current flavivirus vaccine development: a brief review. Viruses. 2023;15(4):860. DOI: https://doi.org/10.3390/v15040860
- Ershova A.S., Gra O.A., Lyaschuk A.M., et al. Recombinant domains III of Tick-Borne Encephalitis Virus envelope protein in combination with dextran and CpGs induce immune response and partial protectiveness against TBE virus infection in mice. BMC Infect. Dis. 2016;16(1):544. DOI: https://doi.org/10.1186/s12879-016-1884-5
- Zhang M., Jin H., Jiao C., et al. An effective tick-borne encephalitis virus vaccine candidate based on virus-like particles induced specific cellular and humoral immunity in mice. 2023. Preprint. DOI: https://doi.org/10.2139/ssrn.4528843
- Tang J., Fu M., Xu C., et al. Development of a novel virus-like particle-based vaccine for preventing tick-borne encephalitis virus infection. Virol. Sin. 2023;38(5):767–77. DOI: https://doi.org/10.1016/j.virs.2023.06.003
- Beicht J., Kubinski M., Zdora I., et al. Induction of humoral and cell-mediated immunity to the NS1 protein of TBEV with recombinant Influenza virus and MVA affords partial protection against lethal TBEV infection in mice. Front. Immunol. 2023;14:1177324. DOI: https://doi.org/10.3389/fimmu.2023.1177324
- Kubinski M., Beicht J., Zdora I., et al. A recombinant Modified Vaccinia virus Ankara expressing prME of tick-borne encephalitis virus affords mice full protection against TBEV infection. Front. Immunol. 2023;14:1182963. DOI: https://doi.org/10.3389/fimmu.2023.1182963
- Li A., Yu J., Lu M., et al. A Zika virus vaccine expressing premembrane-envelope-NS1 polyprotein. Nat. Commun. 2018; 9(1):3067. DOI: https://doi.org/10.1038/s41467-018-05276-4
- Nürnberger C., Bodmer B.S., Fiedler A.H., et al. A measles virus-based vaccine candidate mediates protection against Zika virus in an allogeneic mouse pregnancy model. J. Virol. 2019;93(3): e01485-18. DOI: https://doi.org/10.1128/JVI.01485-18
- Kisakov D.N., Kisakova L.A., Borgoyakova M.B., et al. Optimization of in vivo electroporation conditions and delivery of DNA vaccine encoding SARS-CoV-2 RBD using the determined protocol. Pharmaceutics. 2022;14(11):2259. DOI: https://doi.org/10.3390/pharmaceutics14112259.
- Li L., Petrovsky N. Molecular mechanisms for enhanced DNA vaccine immunogenicity. Expert Rev. Vaccines. 2016;15(3):313–29. DOI: https://doi.org/10.1586/14760584.2016.1124762
- Aberle J.H., Aberle S.W., Kofler R.M., Mandl C.W. Humoral and cellular immune response to RNA immunization with flavivirus replicons derived from tick-borne encephalitis virus. J. Virol. 2005;79(24):15107-13. DOI: https://doi.org/10.1128/JVI.79.24.15107-15113.2005
- Kofler R.M., Aberle J.H., Aberle S.W., et al. Mimicking live flavivirus immunization with a noninfectious RNA vaccine. Proc. Natl Acad. Sci. USA. 2004;101(7):1951–6. DOI: https://doi.org/10.1073/pnas.0307145101
- Wollner C.J., Richner J.M. mRNA vaccines against flaviviruses. Vaccines (Basel). 2021; 9(2):148. DOI: https://doi.org/10.3390/vaccines9020148
- Omori-Urabe Y., Yoshii K., Ikawa-Yoshida A., et al. Needle-free jet injection of DNA and protein vaccine of the far-eastern subtype of tick-borne encephalitis virus induces protective immunity in mice. Microbiol. Immunol. 2011;55(12):893–7. DOI: https://doi.org/10.1111/j.1348-0421.2011.00389.x
- Aberle J.H., Aberle S.W., Allison S.L., et al. A DNA immunization model study with constructs expressing the tick-borne encephalitis virus envelope protein E in different physical forms. J. Immunol. 1999;163(12):6756–61.
- Korber B., Fischer W. T cell-based strategies for HIV-1 vaccines. Hum. Vaccin. Immunother. 2020;16(3):713–22. DOI: https://doi.org/10.1080/21645515.2019.1666957
- Vita R., Mahajan S., Overton J.A., et al. The Immune Epitope Database (IEDB): 2018 update. Nucleic Acids Res. 2019; 47(D1):D339-43. DOI: https://doi.org/10.1093/nar/gky1006
- Antonets D.V., Bazhan S.I. PolyCTLDesigner: a computational tool for constructing polyepitope T-cell antigens. BMC Res. Notes. 2013;6:407. DOI: https://doi.org/10.1186/1756-0500-6-407
- Ezzemani W., Windisch M.P., Altawalah H., et al. Design of a multi-epitope Zika virus vaccine candidate — an in-silico study. J. Biomol. Struct. Dyn. 2023;41(9):3762–71. DOI: https://doi.org/10.1080/07391102.2022.2055648
- Fadaka A.O., Sibuyi N.R.S., Martin D.R., et al. Immunoinformatics design of a novel epitope-based vaccine candidate against dengue virus. Sci. Rep. 2021;11(1):19707. DOI: https://doi.org/10.1038/s41598-021-99227-7
- Nguyen TL, Kim H. Immunoinformatics and computational approaches driven designing a novel vaccine candidate against Powassan virus. Sci. Rep. 2024;14(1):5999. DOI: https://doi.org/10.1038/s41598-024-56554-9
- Choi H., Kudchodkar S.B., Ho M., et al. A novel synthetic DNA vaccine elicits protective immune responses against Powassan virus. PLoS Negl. Trop. Dis. 2020;14(10):e0008788. DOI: https://doi.org/10.1371/journal.pntd.0008788
- Khan N.T., Zinnia M.A., Islam A.B.M.M.K. Modeling mRNA- based vaccine YFV.E1988 against yellow fever virus E-protein using immuno-informatics and reverse vaccinology approach. J. Biomol. Struct. Dyn. 2023;41(5):1617–38. DOI: https://doi.org/10.1080/07391102.2021.2024253
- Borgoyakova M.B., Volosnikova E.A., Ilyichev A.A., Karpenko L.I. Approaches to improve the immunogenicity of plasmid DNA-based vaccines against COVID-19. In: Population Genetics — From DNA to Evolutionary Biology. IntechOpen; 2023. DOI: https://doi.org/10.5772/intechopen.113945
- Боргоякова М.Б., Карпенко Л.И., Рудометов А.П. и др. Искусственный Т-клеточный иммуноген против COVID-19. Бюллетень экспериментальной биологии и медицины. 2023;175(6):767–72. Borgoyakova M.B., Karpenko L.I., Rudometov A.P., et al. Artificial COVID-19 T-cell immunogen. Bulletin of Experimental Biology and Medicine. DOI: https://doi.org/10.47056/0365-9615-2023-175-6-767-772 EDN: https://elibrary.ru/ccsroy
- Chakraborty A., Bayry J., Mukherjee S. Immunoinformatics approaches in designing vaccines against COVID-19. Methods Mol. Biol. 2023;2673:431–52. DOI: https://doi.org/10.1007/978-1-0716-3239-0_29
- Enayatkhani M., Hasaniazad M., Faezi S., et al. Reverse vaccinology approach to design a novel multi-epitope vaccine candidate against COVID-19: an in silico study. J. Biomol. Struct. Dyn. 2021;39(8):2857–72. DOI: https://doi.org/10.1080/07391102.2020.1756411
- Sarkar B., Ullah M.A., Johora F.T., et al. Immunoinformatics-guided designing of epitope-based subunit vaccines against the SARS Coronavirus-2 (SARS-CoV-2). Immunobiology. 2020;225(3):151955. DOI: https://doi.org/10.1016/j.imbio.2020.151955
- Karpenko L.I., Apartsin E.K., Dudko S.G., et al. Cationic polymers for the delivery of the Ebola DNA vaccine encoding artificial T-cell immunogen. Vaccines (Basel). 2020;8(4):718. DOI: https://doi.org/10.3390/vaccines8040718
- Alizadeh M., Amini-Khoei H., Tahmasebian S., et al. Designing a novel multi epitope vaccine against Ebola virus using reverse vaccinology approach. Sci. Rep. 2022;12(1):7757. DOI: https://doi.org/10.1038/s41598-022-11851-z
- Shankar U., Jain N., Mishra S.K., et al. Mining of Ebola virus genome for the construction of multi-epitope vaccine to combat its infection. J. Biomol. Struct. Dyn. 2022;40(11):4815–31. DOI: https://doi.org/10.1080/07391102.2021.1874529
- Albaqami F.F., Altharawi A., Althurwi H.N., et al. Computational modeling and evaluation of potential mRNA and peptide-based vaccine against Marburg Virus (MARV) to provide immune protection against hemorrhagic fever. Biomed. Res. Int. 2023;2023:5560605. DOI: https://doi.org/10.1155/2023/5560605
- Bazhan S.I., Antonets D.V., Starostina E.V., et al. In silico design of influenza A virus artificial epitope-based T-cell antigens and the evaluation of their immunogenicity in mice. J. Biomol. Struct. Dyn. 2022;40(7):3196-212. DOI: https://doi.org/10.1080/07391102.2020.1845978
- Mia M.M., Hasan M., Ahmed S., Rahman M.N. Insight into the first multi-epitope-based peptide subunit vaccine against avian influenza A virus (H5N6): An immunoinformatics approach. Infect. Genet. Evol. 2022;104:105355. DOI: https://doi.org/10.1016/j.meegid.2022.105355
- Sharma S., Kumari V., Kumbhar B.V., et al. Immunoinformatics approach for a novel multi-epitope subunit vaccine design against various subtypes of Influenza A virus. Immunobiology. 2021;226(2):152053. DOI: https://doi.org/10.1016/j.imbio.2021.152053
- Старостина Е.В., Шарабрин С.В., Рудометов А.П. и др. Иммунный ответ на ДНК- и мРНК-вакцины, кодирующие искусственные иммуногены вируса гриппа. Российский иммунологический журнал. 2022;25(3):321–6. Starostina E.V., Sharabrin S.V., Rudometov A.P., et al. Immune response against DNA- and mRNA vaccines encoding artificial influenza virus immunogens. Russian Journal of Immunology. 2022;25(3):321–6. DOI: https://doi.org/10.46235/1028-7221-1103-IRA EDN: https://elibrary.ru/yuzmag
- Stieh D.J., Barouch D.H., Comeaux C., et al. ASCENT/HVTN118/HPX2003 Study Team. Safety and immunogenicity of Ad26-vectored HIV vaccine with mosaic immunogens and a novel mosaic envelope protein in HIV-uninfected adults: A phase 1/2a study. J. Infect. Dis. 2023;227(8):939–50. DOI: https://doi.org/10.1093/infdis/jiac445
- Карпенко Л.И., Бажан С.И., Богрянцева М.П. и др. Комбинированная вакцина против ВИЧ-1 на основе искусственных полиэпитопных иммуногенов: результаты I фазы клинических испытаний. Биоорганическая химия. 2016;42(2):191–204. Karpenko L.I., Bazhan S.I., Bogryantseva M.P., et al. Results of phase I clinical trials of a combined vaccine HIV-1 based on synthetic polyepitope immunogens. Russian Journal of Bioorganic Chemistry. 2016;42(2):191–204. DOI: https://doi.org/10.7868/S0132342316020068 EDN: https://elibrary.ru/vlpwyv
- Кисаков Д.Н., Антонец Д.В., Шабурова Е.В. и др. ДНК-вакцина, кодирующая искусственный Т-клеточный полиэпитопный иммуноген вируса клещевого энцефалита. Бюллетень экспериментальной биологии и медицины. 2023;176(7):85–9. doi: 10.47056/0365-9615-2023-176-7-85-89 EDN: https://elibrary.ru/jlcmud Kisakov D.N., Antonets D.V., Shaburova E.V., et al. DNA vaccine encoding the artificial T-cell polyepitope immunogen of tick-borne encephalitis virus. Bull. Exp. Biol. Med. 2023;176(1):72–6. DOI: https://doi.org/10.1007/s10517-023-05970-4
Supplementary files